Melanoma is one of the most aggressive and deadly types of skin cancer, accounting for 75% of all skin cancer-related deaths despite being less common than basal cell carcinoma or squamous cell carcinoma.
The global incidence of melanoma has been rising, with fair-skinned individuals and those living in high UV exposure areas at greater risk. However, early detection and advancements in treatment have improved survival rates significantly.
This article provides a comprehensive guide to melanoma, covering causes, symptoms, diagnosis, treatment, prognosis, prevention, and the latest research advancements.
[signup]
What is Melanoma?
Understanding melanoma is essential before diving into its causes, symptoms, and treatment options.
Definition and Overview
Melanoma is a type of skin cancer originating in melanocytes, the pigment-producing cells in the skin. Unlike basal and squamous cell carcinoma, melanoma is more likely to spread (metastasize) to distant organs if not detected early.
Types of Melanoma
The four major types of cutaneous (skin) melanoma are:
Superficial Spreading Melanoma
- The most common type (approximately 70% of melanoma cases); grows horizontally (radially) before spreading deeper.
- Common locations: torso, legs, arms
Nodular Melanoma
- More aggressive, grows vertically and quickly.
- Common locations: Areas with chronic sun exposure (e.g., scalp, chest, back)
Lentigo Maligna Melaoma
- Slow-growing, typically evolves from brown to black macule with irregular borders; common in older adults.
- Common locations: Chronically sun-damaged skin on the face and neck.
Acral Lentiginous Melaoma
- Uncommon; affects palms, soles, and undernails; disproportionately affects individuals with darker skin tones.
- Common locations: Hands, feet, nail beds
Early detection and treatment significantly improve prognosis and survival rates.
Global Incidence Rates
The reported incidence varies by region due to differences in UV exposure, genetic susceptibility, and healthcare access. Some populations may have lower documented cases due to differences in screening practices and reporting accuracy. Typically:
- Australia and New Zealand have the highest melanoma rates globally due to high UV exposure and fair-skinned populations.
- North America and Europe see moderate incidence rates, with increasing cases due to tanning practices.
- Asia and Africa have lower reported cases, though acral lentiginous melanoma is more common in darker-skinned individuals.
Causes and Risk Factors
Melanoma is multifactorial, resulting from a combination of genetic, environmental, and lifestyle influences.
Genetic Factors
- A family history of melanoma increases risk 2-3 times.
- Mutations in genes like CDKN2A and BRAF are associated with an increased risk of melanoma.
- Hereditary syndromes like familial atypical multiple mole melanoma (FAMMM) syndrome increase susceptibility.
Environmental Factors
- UV radiation (sunlight & tanning beds) damages DNA, leading to cancerous mutations.
- Higher risk in sunny climates (Australia, southern U.S., and Mediterranean regions).
Lifestyle Factors
- Frequent sunburns in childhood increase melanoma risk later in life.
- Occupational exposures (e.g., outdoor jobs) elevate risk.
Rare Causes
- Weakened immune system (due to organ transplants, chemotherapy, or autoimmune diseases).
- Certain medications, including immunosuppressants, may be associated with an increased susceptibility to melanoma.
Symptoms and Signs
Recognizing the early signs of melanoma is crucial for early detection and better treatment outcomes.
Common Symptoms
- Changes in mole size, shape, or color.
- New, abnormal skin growths.
- Irregular borders, multiple colors, or asymmetry in a mole.
Less common symptoms include moles that itch, bleed, or become tender and sores that do not heal.
How to Perform a Self-Examination
To perform a skin self-examination at home:
- Start by standing in a well-lit room with a full-length mirror and a hand-held mirror.
- Begin by examining your entire body, including your face, neck, chest, and abdomen. Women should also check under their breasts.
- Next, inspect both arms, including your hands, nails, and between your fingers.
- Sit down and examine your legs, feet (including soles and between toes), and toenails.
- Use a hand-held mirror to check hard-to-see areas such as your back, buttocks, and the back of your neck and scalp.
Look for new, changing, or unusual moles, spots, or lesions using the ABCDE rule - Asymmetry, Border irregularity, Color variation, Diameter over 6mm, and Evolution (Table 1). If you notice any suspicious changes, consult a dermatologist promptly.
Follow the ABCDE rule for detecting suspicious moles
Detecting Suspicious Moles

Diagnosis of Melanoma
Early diagnosis is crucial for the best treatment outcomes.
Early Detection Methods
Early detection of melanoma significantly improves treatment success and survival rates. Regular self-exams can help detect suspicious skin changes, but professional dermatologic evaluation is necessary for an accurate diagnosis.
- Self-Exams: Individuals should check their skin monthly, looking for new or changing moles using the ABCDE rule (Asymmetry, Border irregularity, Color variation, Diameter >6mm, and Evolving appearance).
- Dermatology Visits: People at higher risk (family history, fair skin, history of sunburns, or many moles) should have a yearly full-body skin exam by a dermatologist (a doctor specializing in diagnosis and treatment of conditions of the skin, hair, and nails).
- Dermatoscopy (Epiluminescence Microscopy): A non-invasive imaging tool that magnifies skin lesions to assess suspicious moles more closely, helping dermatologists decide if a biopsy is needed.
Advanced Diagnostic Procedures
If a suspicious lesion is identified, a biopsy should be performed to determine whether it is melanoma. Biopsy methods include:
- The entire mole and a small margin of normal skin are removed for lab testing.
- Preferred for most suspicious moles.
- A portion of the lesion is removed for analysis.
- Used if the lesion is too large for full removal.
- A circular tool removes a small, deep sample.
- Used when deeper tissue examination is required.
- The top layers of the skin are removed.
- Shave biopsy is generally not preferred for suspected melanoma but may be considered in select cases.
Imaging Tests for Advanced Melanoma
If melanoma is suspected to have spread beyond the skin, imaging tests may be ordered:
- CT Scans & MRI: Useful in melanoma assessment to detect metastases, evaluate tumor depth, and assess the involvement of lymph nodes or internal organs, aiding in staging and treatment planning.
- PET Scan: Assess metabolically active cancer cells, allowing for the identification of distant metastases and assessment of disease progression.
Staging Melanoma
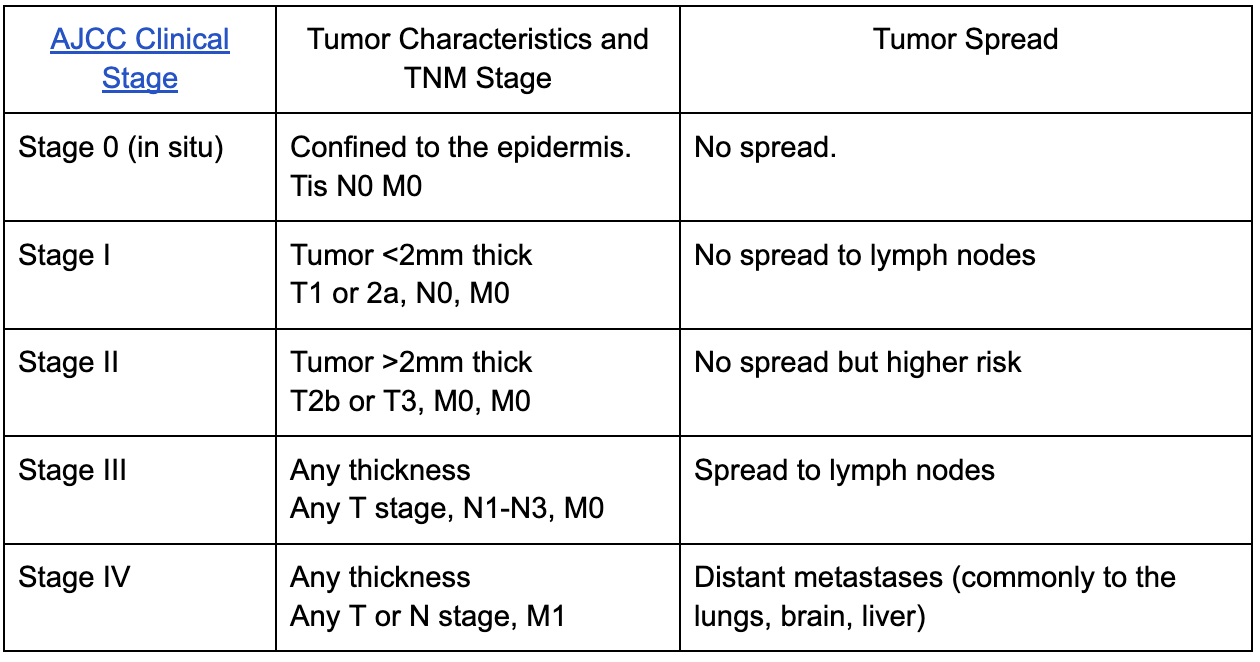
After diagnosis, melanoma is staged using the TNM (Tumor, Nodes, Metastasis) staging system to guide treatment decisions (Table 2). Treatment strategies vary based on the severity and spread of the disease.
Melanoma Staging
Differential Diagnosis
The differential diagnosis for melanoma includes skin lesions that may appear similar. For example:
- Atypical fibroxanthoma
- Pigmented basal cell carcinoma
- Blue nevus
- Epithelioid tumor
- Halo nevus
A definitive melanoma diagnosis requires histopathological evaluation by a qualified pathologist.
Treatment Options
Melanoma treatment depends on stage, location, patient health, and genetic factors. Earlier-stage melanomas are often curable with surgery, while advanced cases may require systemic therapies like immunotherapy or targeted therapy.
Conventional Treatments
Surgical Removal (Excision or Mohs Surgery)
- Stage 0 to II melanoma is treated with wide excision, where the tumor and a margin of surrounding healthy tissue are removed.
- Mohs micrographic surgery is used for certain melanomas on the face or sensitive areas, allowing layer-by-layer removal while preserving healthy tissue.
- Lymph Node Dissection: If melanoma has spread to regional lymph nodes, surgical removal may be needed.
Radiation Therapy
- Used after surgery for high-risk cases to eliminate residual cancer cells.
- Also used palliatively for metastatic melanoma that has spread to the brain, bones, or other organs.
Chemotherapy
- Previously a main treatment for advanced melanoma, chemotherapy is now used less frequently due to the success of immunotherapy and targeted therapies.
Advanced Treatments
Recent breakthroughs in melanoma treatment have led to more effective therapies with improved survival rates.
Immunotherapy (Checkpoint Inhibitors)
- Boosts the immune system’s ability to attack melanoma cells.
- Common drugs:
- Pembrolizumab (Keytruda), Nivolumab (Opdivo): PD-1 inhibitors that block immune suppression.
- Ipilimumab (Yervoy): A CTLA-4 inhibitor that enhances T-cell activation.
- For patients with BRAF mutations (50% of melanomas):
- BRAF inhibitors: Vemurafenib, Dabrafenib.
- MEK inhibitors: Trametinib, Cobimetinib.
- These drugs shrink tumors and slow the progression of advanced melanoma.
Combination Therapy
- Using immunotherapy and targeted therapy together has shown promising results in improving survival.
Treatment Based on Stage

Effective treatment improves survival rates, but prognosis depends on factors such as tumor thickness and metastasis.
Prognosis and Survival Rates
Factors Affecting Prognosis
Several factors influence melanoma prognosis:
- Tumor Thickness: Thicker tumors have a higher chance of spreading and a worse prognosis.
- Ulceration: If the tumor breaks through the skin, the prognosis worsens.
- Lymph Node Involvement: The more lymph nodes affected, the lower the survival rate.
- Distant Metastasis: Stage IV melanoma has the lowest survival rate, especially if it spreads to the brain or liver.
Prevention and Risk Reduction
Adopting protective measures can significantly lower the risk of developing melanoma.
Sun Protection Strategies
Protecting your skin from harmful UV radiation is one of the most effective ways to reduce melanoma risk. Here are some tips:
Use Broad-Spectrum Sunscreen
- The FDA recommends using a broad-spectrum sunscreen with SPF 30 or higher to reduce UV exposure risk.
- Reapply every two hours and immediately after swimming or sweating.
- Choose broad-spectrum formulas that protect against UVA and UVB rays.
Wear Protective Clothing and Accessories
- Wide-brimmed hats, long sleeves, and sunglasses reduce UV exposure.
- Ultraviolet Protection Factor (UPF-rated) clothing provides additional protection.
Avoid Tanning Beds and Excessive Sun Exposure
- Tanning beds emit concentrated UV radiation, increasing melanoma risk. The WHO and FDA classify tanning beds as carcinogenic, with evidence linking them to an increased risk of melanoma.
- Limit direct sun exposure between 10 AM and 4 PM, when UV rays are strongest.
Monitor UV Index and Seek Shade
- Use weather apps to check the daily UV index.
- When UV levels are high, stay in shaded areas and avoid prolonged sun exposure.
Lifestyle Changes for Melanoma Prevention
A healthy lifestyle may lower the risk of developing melanoma. Examples include:
- Antioxidant-Rich Diet: Foods rich in antioxidants (berries, leafy greens, nuts) may help protect skin cells from UV damage. Omega-3 fatty acids from fish may have anti-inflammatory effects that benefit skin health.
- Avoid Smoking and Limit Alcohol
- Maintain a Healthy Immune System: Immunosuppression (due to organ transplants, autoimmune diseases, or chronic illnesses) may increase melanoma risk. Staying physically active and managing stress can support immune function.
Regular Screenings and Dermatological Exams
Routine skin checks are essential in catching melanoma early, when treatment is most effective.
Who Should Get Screened?
- Individuals with a family history of melanoma.
- People with fair skin, freckles, or numerous moles.
- Those with a history of severe sunburns or tanning bed use.
Professional Skin Exams
- Annual dermatologist visits are recommended for high-risk individuals.
- Total-body photography helps track mole changes over time.
Melanoma Research and Future Directions
Medical advancements have transformed melanoma from a high-mortality cancer to one with increasingly better survival rates. Research is focused on enhancing early detection, developing novel treatments, and improving patient outcomes.
Latest Research Findings
- Artificial intelligence (AI) tools are being developed to detect melanoma more accurately in early stages using imaging technology.
- Gene Editing & CRISPR-Based Treatments: Scientists are exploring gene therapy to correct genetic mutations responsible for melanoma.
New Developments in Immunotherapy
- Dual checkpoint inhibitors (combining PD-1 and CTLA-4 blockers) are being studied to enhance immune response further.
- T-cell therapy (adoptive cell transfer) is being investigated to improve treatment for advanced melanoma.
Targeted Therapy Advances
- Next-generation BRAF inhibitors aim to prolong treatment response and reduce drug resistance.
- Combination therapies using targeted drugs and immunotherapy are showing higher survival rates.
Living with Melanoma
Melanoma treatments can cause short-term and long-term side effects. For example:
- Surgery may result in scarring and pain. Scar creams and pain relief medications may help.
- Immunotherapy may cause fatigue, skin rash, and inflammation. Hydration, rest, and managing autoimmunity may provide relief.
- Radiation may cause skin irritation and fatigue. Moisturizers and gentle exercises (yoga, walking, swimming) may help manage treatment-related fatigue.
Support Systems and Resources
Emotional and Mental Health Support
- A melanoma diagnosis can be overwhelming, leading to anxiety or depression.
- Therapy, mindfulness techniques, and patient support groups can help individuals cope.
Support Groups & Online Communities
- The Skin Cancer Foundation provides education and patient advocacy.
- Melanoma Research Alliance offers access to clinical trials and new treatments.
Financial and Practical Assistance
- Nonprofits like the American Cancer Society provide grants and financial aid for treatment costs.
- Transportation services are available for patients who need assistance getting to medical appointments.
After completing treatment, melanoma survivors should follow their healthcare provider’s recommendations for surveillance and follow-up visits.
Understanding melanoma is essential for recognizing risk factors and seeking timely medical care. This article provides general information and should not replace professional medical evaluation or treatment.
[signup]
Key Takeaways
- Melanoma is one of the most aggressive forms of skin cancer, but early detection significantly improves survival rates, with Stage 0 and Stage I cases having a 90-99% survival rate.
- UV radiation exposure is the leading environmental cause, so sunscreen, protective clothing, and avoiding tanning beds are essential for prevention.
- Regular skin checks using the ABCDE rule (Asymmetry, Border irregularity, Color variation, Diameter >6mm, and Evolving changes) help in detecting melanoma early before it spreads.
- Diagnosis is confirmed through biopsy and staging, with advanced imaging (CT, MRI, PET scans) used to detect metastases in later stages.
- Treatment varies by stage—early-stage melanoma is often curable with surgery, while advanced cases may require immunotherapy, targeted therapy, or radiation.
- Immunotherapy and targeted therapy have revolutionized melanoma treatment, particularly for Stage III and IV melanoma, improving survival rates dramatically.
- Ongoing research in genetics, immunotherapy, and artificial intelligence (AI) for early detection is paving the way for more precise, personalized melanoma treatments.
- Survivors require long-term follow-up and lifestyle adjustments, including routine skin exams, sun protection, and emotional support through patient advocacy groups.
Melanoma prevention, early detection, and advances in medical research continue to save lives. Regular screenings, sun-safe habits, and staying informed about treatment options are key to reducing the global burden of this disease.












%201.svg)










