Steroid-induced psychosis is a rare but serious side effect of corticosteroid use, affecting approximately 5-18% of patients receiving high-dose steroid therapy. While corticosteroids are essential for treating inflammatory, autoimmune, and allergic conditions, they can also disrupt brain chemistry, leading to psychiatric symptoms, including mood swings, anxiety, paranoia, and hallucinations.
This article explores the causes, symptoms, diagnosis, treatment, and prevention of steroid-induced psychosis.
[signup]
Understanding Steroid-Induced Psychosis
Psychiatric side effects of corticosteroids can range from mild mood changes to severe psychotic symptoms. While most cases resolve after discontinuation or dose reduction, Early recognition and management may help reduce the severity of symptoms and improve outcomes.
Definition and Prevalence
Steroid-induced psychosis refers to psychotic symptoms (e.g., hallucinations, delusions, disorganized thinking) that may develop in some individuals by the use of corticosteroids, such as prednisone, dexamethasone, and methylprednisolone.
Pathophysiology: How Do Steroids Cause Psychosis?
Steroids alter brain chemistry, potentially increasing the risk of mood instability, hallucinations, and cognitive impairment. Corticosteroids affect brain function through several mechanisms:
- Hypothalamo-Pituitary-Adrenal (HPA) Axis Dysfunction: Disrupts stress response and increases cortisol levels.
- Neurotransmitter Imbalance: Alters dopamine and serotonin levels, which regulate mood and perception.
- Glutamate Excitotoxicity: Excessive glutamate activity can cause cognitive and emotional instability.
Risk Factors for Steroid-Induced Psychosis
While anyone taking corticosteroids can experience psychiatric side effects, some individuals are at higher risk.
- Higher Dosage & Long-Term Use: Higher steroid doses correlate with a greater risk of psychiatric symptoms.
- Pre-existing Psychiatric Conditions: Patients with bipolar disorder, schizophrenia, or major depression are at increased risk.
- Age & Gender: Some studies suggest that elderly patients and women may have a higher likelihood of experiencing psychiatric side effects from steroids, but individual risk varies.
Clinical Manifestations
Steroid-induced psychosis can present in various ways, from mild mood swings to severe delusions and hallucinations. Recognizing early warning signs can help prevent progression to full-blown psychosis.
Early Warning Signs
Before psychosis develops, patients may experience:
- Sudden mood changes: Feeling unusually euphoric, irritable, or emotionally unstable.
- Sleep disturbances: Insomnia or disrupted sleep cycles.
- Increased restlessness or anxiety: Feeling overwhelmed or excessively worried.
Psychiatric Symptoms
Steroid-induced psychosis can mimic other mental health disorders, including bipolar disorder, depression, and anxiety disorders. For example:
- Manic Symptoms: Excessive energy, racing thoughts, impulsivity
- Depressive Symptoms: Low mood, hopelessness, suicidal thoughts
- Severe Anxiety: Panic attacks, paranoia, agitation
Patients with rapid-onset mood changes or severe anxiety while on steroids should seek medical evaluation.
Psychotic Features
In some cases, steroid-induced psychosis may involve hallucinations, delusions, or cognitive impairment, though symptom severity varies among individuals.
- Hallucinations: Seeing, hearing, or feeling things that aren’t real.
- Delusions: Fixed, false beliefs (e.g., paranoia, grandiosity).
- Cognitive Impairment: Confusion, disorganized thinking, and memory loss.
Timeline of Symptom Onset
Symptoms can appear rapidly, especially in high-dose steroid users.
- Mood disturbances: Typically onset within days.
- Anxiety or panic attacks: 1-2 weeks
- Hallucinations and delusions: 1-4 weeks (high-dose users)
Diagnosis and Assessment
Proper diagnosis of steroid-induced psychosis is essential to differentiate it from primary psychiatric disorders or other medical conditions that can cause similar symptoms.
Diagnostic Criteria
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies steroid-induced psychosis under substance/medication-induced mental disorders if:
- Psychotic symptoms (hallucinations, delusions, cognitive dysfunction) appear after initiating corticosteroids.
- Symptoms are not better explained by an underlying psychiatric condition (e.g., schizophrenia, bipolar disorder).
- The symptoms cause significant distress or impairment in daily life.
A diagnosis of steroid-induced psychosis requires clear evidence that symptoms are directly linked to steroid use and not a separate psychiatric condition.
Clinical Evaluation
A detailed patient history and physical examination are critical for diagnosing steroid-induced psychosis.
Psychiatric History:
- Previous mental health disorders (bipolar disorder, schizophrenia, anxiety, depression).
- Family history of psychiatric conditions.
- Prior experiences with corticosteroids and psychiatric symptoms.
Mental Status Examination (MSE):
- Appearance and behavior: Agitation, restlessness, or confusion.
- Mood and affect: Signs of mania, depression, or emotional instability.
- Thought processes: Disorganized thinking, paranoia, delusions.
- Perception: Presence of hallucinations (visual or auditory).
Laboratory Tests & Metabolic Screening:
- Electrolyte imbalances (low sodium, high calcium) may contribute to psychiatric symptoms.
- C-reactive protein (CRP) and inflammatory markers can assess ongoing systemic inflammation.p
- Thyroid function tests to rule out hyperthyroidism-induced psychiatric effects.
Neuroimaging and Other Diagnostic Tools
In some cases, additional assessments may be required to exclude other causes of psychotic symptoms. For example:
- Computed Tomography (CT) or Magnetic Resonance Imaging (MRI): Used to help rule out brain lesions, tumors, or strokes that may mimic psychosis.
- Positron Emission Tomography (PET) Scan: Assess brain metabolism in severe or persistent cases.
- Electroencephalogram (EEG): Identifies seizure-related causes of psychiatric symptoms.
Treatment Approaches
Lowering the steroid dose is often the first approach to managing symptoms, but some individuals may require additional psychiatric support or medication.
Steroid Management: Adjusting Medication Safely
The first and most effective treatment for steroid-induced psychosis is reducing or discontinuing corticosteroid therapy when possible.
Tapering Strategies:
- Gradual dose reduction instead of abrupt discontinuation to avoid adrenal insufficiency.
- If tapering is not an option, switching to a lower-dose or alternative anti-inflammatory medication may help.
Steroid Altrnatives:
- Non-steroidal immunosuppressants (e.g., methotrexate, azathioprine, hydroxychloroquine) in autoimmune diseases.
- Biologic therapies (TNF inhibitors, monoclonal antibodies) for inflammatory conditions.
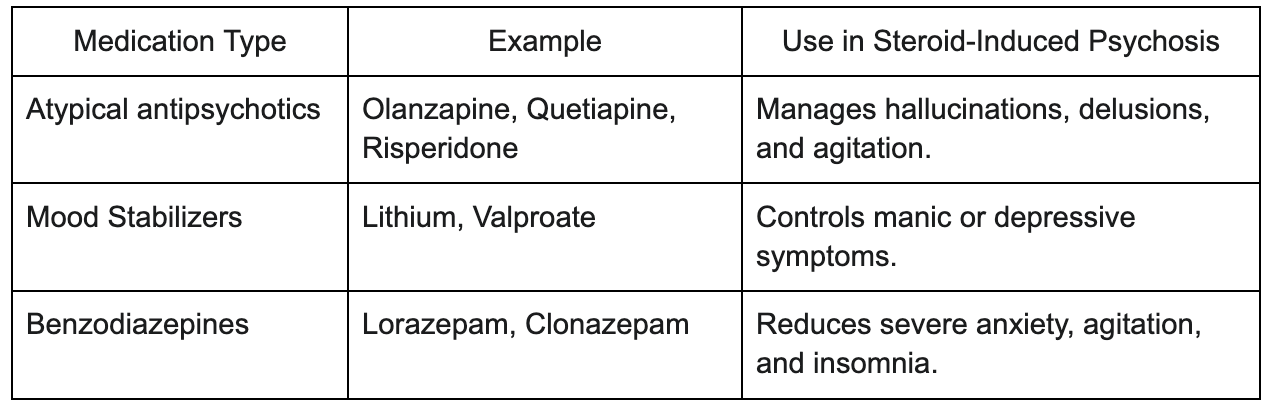
Pharmacological Interventions
For patients experiencing severe psychosis, mood instability, or hallucinations, psychiatric medications may be necessary while steroids are tapered. Commonly used medications are listed in Table 1.
Psychotherapy and Supportive Care
In addition to medication, counseling and social support play a key role in helping patients recover.
- Cognitive Behavioral Therapy (CBT): Helps patients manage anxiety, paranoia, and mood instability.
- Family Education and Support Groups: Caregivers should know potential symptoms and treatment strategies.
Prevention and Monitoring
Not all patients on steroids will develop psychiatric symptoms; proactive screening and monitoring help identify high-risk individuals early.
Risk Assessment Before Starting Steroid Therapy
Before prescribing steroids, healthcare providers should:
- Screen for psychiatric vulnerabilities: Evaluate patients for a history of depression, anxiety, or bipolar disorder.
- Discuss potential side effects: Patients should be educated about mood and behavior changes.
- Evaluate alternative treatments: Use the lowest effective dose of steroids for the shortest duration possible.
Monitoring During Steroid Treatment
Close monitoring can help detect early symptoms of steroid-induced psychosis.
- Regular mental health check-ins with a healthcare provider: Monitor for mood swings, paranoia, or sleep disturbances.
- Early intervention strategies: Reduce dose at first sign of psychiatric distress.
- Patient and caregiver education: Encourage self-reporting of unusual symptoms.
Ongoing monitoring ensures early detection and timely management of symptoms.
Long-Term Follow-Up
Even after stopping steroids, some patients may experience lingering psychiatric effects.
- Post-treatment psychiatric evaluations: Ensure full resolution of symptoms.
- Relapse prevention strategies: Alternative medications for future inflammatory conditions.
Special Populations and Considerations
While steroid-induced psychosis can occur in anyone taking corticosteroids, certain populations are more vulnerable due to age-related factors, underlying health conditions, or pre-existing psychiatric disorders. Special considerations must be made to minimize risks and ensure proper management.
Pediatric Patients: Unique Challenges and Considerations
Children and adolescents prescribed corticosteroids for conditions like asthma, autoimmune diseases, or organ transplants may be at higher risk for behavioral and mood disturbances due to their developing nervous systems.
Common Symptoms in Pediatric Patients:
- Irritability, hyperactivity, and emotional outbursts
- Severe mood swings that may be mistaken for normal childhood behavior
- Cognitive effects such as difficulty concentrating or forgetfulness
Long-Term Neurodevelopmental Concerns
Pediatric patients should be monitored closely for mood changes, and steroid doses should be kept as low as possible while balancing medical needs. Prolonged steroid use in children may impact:
- Brain development: Long-term steroid use in children has raised concerns about potential effects on neurodevelopment, though more research is needed to fully understand the impact.
- Social behavior and academic performance: Mood instability can affect school performance and peer interactions.
Elderly Patients: Increased Susceptibility and Risks
Older adults are particularly prone to steroid-induced psychiatric symptoms, including delirium, confusion, and hallucinations. This is due to age-related changes in brain function and increased sensitivity to medications.
Common Symptoms in Elderly Patients:
- Memory problems or sudden cognitive decline
- Increased risk of delirium (especially in hospitalized patients)
- Mood instability, depression, or withdrawal from social interactions
Medication Interactions and Dosage Adjustments
Elderly patients often take multiple medications, which increases the risk of drug interactions. Special care should be taken to:
- Avoid high-dose steroids whenever possible.
- Adjust steroid doses based on kidney and liver function to prevent accumulation and toxicity.
- Monitor for interactions with antidepressants, antipsychotics, and blood pressure medications.
Lower steroid doses and careful medication management are essential in elderly patients to minimize psychiatric risks.
Patients with Pre-existing Psychiatric Conditions: High-Risk Management
Patients with bipolar disorder, schizophrenia, major depression, or anxiety disorders are at higher risk of developing severe steroid-induced psychiatric symptoms. Even at low doses, steroids may exacerbate mood disorders, trigger mania, or lead to psychotic episodes.
Management Strategies for High-Risk Patients
- Pre-treatment psychiatric screening: Identify patients at high risk before starting steroids.
- Collaborative care: Work with a healthcare provider or psychiatrist to adjust medications if needed.
- Lower doses or alternative treatments: Minimize steroid use whenever possible.
Psychiatric symptoms may appear more rapidly and severely in individuals with pre-existing mental health conditions, requiring proactive monitoring and intervention.
Future Directions and Research
Ongoing research aims to better understand steroid-induced psychosis and develop safer treatments with fewer psychiatric side effects. Scientists are focusing on new medications, genetic risk factors, and personalized treatment approaches to minimize risks.
Emerging Therapies: Safer Anti-Inflammatory Options
New drug development focuses on reducing the need for high-dose corticosteroids by introducing safer alternatives:
- Non-steroidal immunosuppressants: Drugs like methotrexate, azathioprine, and mycophenolate mofetil offer inflammation control with lower psychiatric risks.
- Biologic therapies: TNF inhibitors, IL-6 blockers, and monoclonal antibodies are being developed to treat autoimmune diseases without triggering psychiatric effects.
- Neuroprotective strategies: Some studies suggest that supplements like omega-3 fatty acids and N-acetylcysteine (NAC) may protect against corticosteroid-related brain changes, but more research is needed to determine their effectiveness in preventing steroid-related psychiatric symptoms.
Genetic and Biomarker Research: Identifying High-Risk Individuals
Researchers are exploring genetic and biological markers that may predict who is most vulnerable to steroid-induced psychosis.
Potential Genetic Factors:
- Variants in dopamine, serotonin, and cortisol-related genes may influence how the brain reacts to steroids.
- Some studies suggest that individuals with a family history of mood disorders may be genetically predisposed to psychiatric side effects.
Biomarkers in Blood Tests:
- Inflammatory markers (IL-6, TNF-α) may correlate with higher psychiatric risk.
- Cortisol levels and HPA axis function may help predict who will develop mood or psychotic symptoms.
Improving Clinical Guidelines: Toward Better Prevention and Management
As new research emerges, clinical guidelines for prescribing corticosteroids are evolving. Future recommendations may include:
- Routine psychiatric screening before starting steroids: Identifying at-risk individuals before symptoms develop.
- Standardized tapering protocols: Optimizing how steroids are reduced to minimize withdrawal effects.
- Improved education for patients and healthcare providers: Ensuring that both doctors and patients understand the risks and warning signs of steroid-induced psychosis.
[signup]
Key Takeaways
- Steroid-induced psychosis is a rare but serious side effect of corticosteroid use, especially at high doses (above 40 mg/day) or with long-term use.
- Symptoms can include mood swings, anxiety, paranoia, hallucinations, and delusions. Early signs often involve insomnia, irritability, and emotional instability before progressing to more severe symptoms.
- Higher doses and longer-acting steroids (e.g., prednisone, dexamethasone) carry the highest risk, while inhaled or topical steroids rarely cause psychiatric symptoms.
- Most cases resolve within days to weeks after stopping or reducing the steroid dose, but some individuals may need medications like antipsychotics or mood stabilizers for symptom control.
- Pre-existing mental health conditions, advanced age, and prolonged steroid use increase the risk of developing steroid-induced psychosis. Screening and close monitoring are critical for high-risk patients.
- Psychotherapy, family support, and patient education play important roles in managing and preventing steroid-induced psychiatric symptoms.
- New research is exploring genetic risk factors and alternative anti-inflammatory treatments to reduce the likelihood of psychiatric side effects from steroids.
- Healthcare providers should assess psychiatric history before prescribing steroids and educate patients on potential mental health side effects to ensure early detection and intervention.












%201.svg)









