Artificial Intelligence (AI) is rapidly changing the field of medicine, impacting how diagnosis, treatment planning, patient care management, and clinical research are performed. By implementing the use of AI in the clinical care setting, clinicians can analyze complex medical data with faster speed and greater accuracy. This article aims to explore the current and future applications of AI in healthcare. AI-related barriers and ethical considerations will also be presented.
Before we discuss AI’s role in health care, it is helpful to know the basics about AI. AI is based on the foundations of machine learning and deep learning. Machine learning enables computers to take large datasets and create statistical algorithms. Deep learning is a subset of machine learning that uses neural networks to analyze and interpret vastly complex data structures.
Deep learning is particularly useful in image analysis for the detection of various health conditions. AI can rapidly process and analyze data from vastly large datasets, such as from 50,000+ electronic medical records, including medical images, and genomic sequences, and output patterns and trends in patient data, surpassing the speed and ability of the human brain and traditional software. The results foster greater efficiency of patient care, early disease detection, accurate diagnosis, improved cost-efficiency of healthcare delivery, and clinical research.
[signup]
Applications of AI in Healthcare
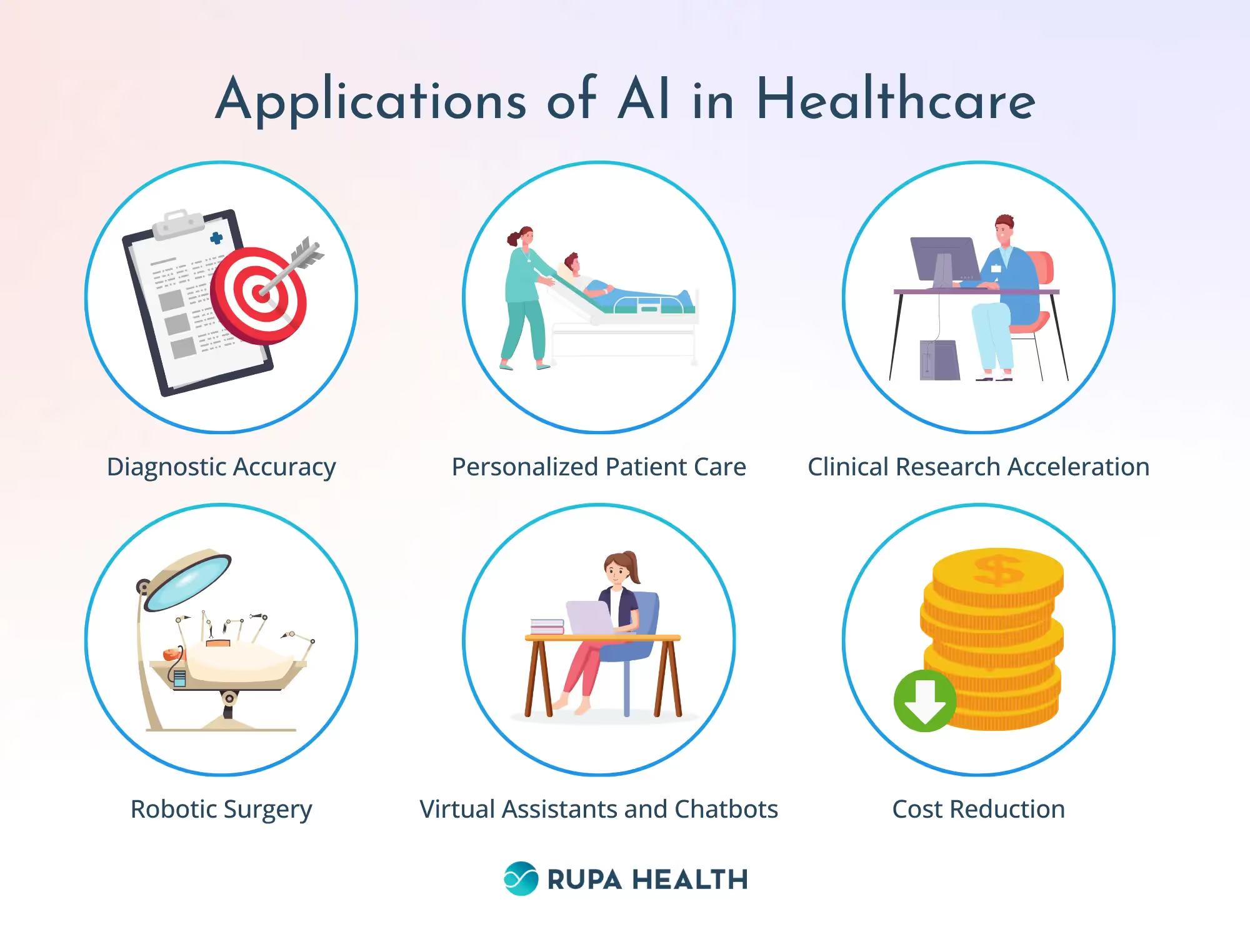
The role of AI in medicine and healthcare is quickly expanding. Some of its current roles include:
1) Enhancing diagnostic accuracy through advanced image analysis techniques in radiology, pathology, and dermatology. Machine learning algorithms can identify patterns in imaging data that may be imperceptible to the human eye, leading to earlier detection and more precise diagnosis of several conditions. One example is the use of an AI image-based program that evaluates the mouth, larynx, and trachea for potential complications during intubation for general anesthesia. Having this information before intubation allows the anesthesiologist to plan ahead and potentially modify the manner intubation or ventilation may be done for a surgical procedure to avoid complications. As another example, AI has shown remarkable proficiency in diagnosing skin conditions, often surpassing the accuracy of experienced dermatologists.
2) AI enhances personalized patient care by analyzing individual genetic, clinical, and lifestyle data to tailor treatments. This precision approach leads to more effective selection of first-line therapies with fewer side effects, improving patient outcomes and satisfaction. AI-driven personalized medicine optimizes treatment plans, ensuring patients receive the most suitable interventions for their unique health profiles.
3) AI significantly accelerates clinical research and development by analyzing large datasets to identify potential drug candidates, predict their efficacy, and optimize clinical trial designs. AI-driven algorithms can streamline the drug discovery process, reducing costs and increasing success rates.
4) AI plays a pivotal role in robotic surgery by enhancing precision, accuracy, and efficiency. Cognitive robotic surgical systems can analyze real-time data, guide complex decision-making, and provide surgeons with augmented visualization. This leads to smaller, more anatomically accurate incisions, reduced human error, reduced operative times, and improved patient outcomes. AI also enables the automation of certain surgical tasks, allowing for minimally invasive procedures with quicker recovery times. As an example, an integrated AI-robotic system can guide the surgeon to make quick decisions when a patient’s anatomy differs from textbook anatomy, such as in a patient with situs inversus.
5) AI-powered virtual assistants and chatbots offer patient support and operational efficiencies by providing appointment and health-related reminders, answering health-related queries, and monitoring and triaging symptoms. These tools improve patient engagement, patient satisfaction, and adherence to treatment plans, and reduce patient wait times.
6) AI has helped reduce healthcare costs by enhancing diagnostic accuracy, streamlining operations, and enabling preventive care. AI-driven tools improve efficiency, minimizing unnecessary tests and procedures, and leading to earlier interventions that prevent costly complications. By optimizing resource allocation and treatment plans, AI contributes to more cost-effective healthcare delivery.
Challenges and Ethical Considerations
The implementation of AI in healthcare presents several challenges that need to be addressed to ensure its ethical and effective integration. One area of concern is data privacy, as the use of AI relies on vast amounts of personal health data, which raises concerns about privacy and data security. Additionally, there are ethical implications associated with cost-related AI decision-making processes. For example, most health insurance companies now use AI-based algorithms to make resource allocation decisions such as coverage for various medical procedures. The algorithms used for this purpose are often proprietary, eliminating or reducing transparency in AI algorithms, often referred to as the "black box" issue. These algorithms need to be transparent to ensure that their decision-making processes are fair, unbiased, and understandable to both patients and healthcare providers.
Another challenge is unintentional bias in AI. Bias in AI algorithms for health care can have significant consequences by resulting in misdiagnosing certain patient groups, like gender and ethnic minorities. For example, it is well known that cardiovascular disease has different patterns of expression in men versus women, however, an AI algorithm that has been trained with data samples primarily of men may not be as accurate in diagnosing women. Similarly, statistical bias in an AI algorithm used for the design of a clinical trial may skew the results.
The impact of AI on the healthcare workforce cannot be overlooked. The introduction of AI technologies may lead to concerns about job displacement and the need for new training. Managing this transition and ensuring that healthcare professionals are equipped with the necessary skills to work alongside AI technologies is crucial.
The Future of AI in Healthcare
Emerging trends and prospects for Artificial Intelligence in medicine are paving the way for transformative advancements in healthcare. One of the most promising areas is genomics, where AI has the potential to unlock new understanding of genetic disorders and personalized medicine. By analyzing vast amounts of genomic data, AI algorithms can identify patterns and mutations that may be linked to specific diseases, leading to more targeted and effective treatments.
Another significant trend is the enhancement of remote patient monitoring through AI-powered technologies. Wearable devices and sensors equipped with AI algorithms can continuously track vital signs, detect abnormalities, and provide real-time feedback to both patients and healthcare providers. This improves the management of chronic conditions and enables timely interventions.
Furthermore, AI has the potential to foster global health equity by making advanced medical technologies more accessible to underserved populations. For example, AI-driven diagnostic tools can be deployed in remote areas with limited healthcare infrastructure, providing critical medical insights that would otherwise be unavailable.
[signup]
Key Takeaways
The implementation of AI in medicine offers groundbreaking opportunities to enhance diagnostics, personalize treatments, cost-efficacy, patient outcomes, and improve healthcare accessibility. However, realizing the full benefits of AI in healthcare requires ongoing innovation, ethical considerations, training of the healthcare workforce, and collaborative efforts among healthcare professionals, technologists, and policymakers.
Addressing challenges such as data privacy, decision-making transparency, and workforce impact is crucial to ensure the responsible and equitable integration of AI in medical practice. The role of AI in medicine is growing and its potential to reshape healthcare is limited only by our imaginations.












%201.svg)











