Gastrointestinal disorders are common in children. These disorders can significantly limit a child's quality of life, act as a source of distress for children and their caregivers, and negatively impact the child's growth and risk for future health issues. An estimated five million children die annually from the consequences of persistent diarrhea, childhood constipation prevalence rates range from 0.5-32.2%, and irritable bowel syndrome affects up to 14% and 35.5% of children and adolescents, respectively. (53)
Integrative medicine blends conventional medical treatments with complementary therapies like dietary adjustments, natural supplements, and mindfulness practices. This holistic strategy addresses not just physical symptoms, but also the emotional and social aspects of these often-complex conditions, potentially supporting improved gut health.
[signup]
Overview of Common Pediatric Digestive Disorders
Understanding common digestive disorders in children, their symptoms, and options for support can empower parents and caregivers to seek timely help for their little ones experiencing gastrointestinal (GI) symptoms.
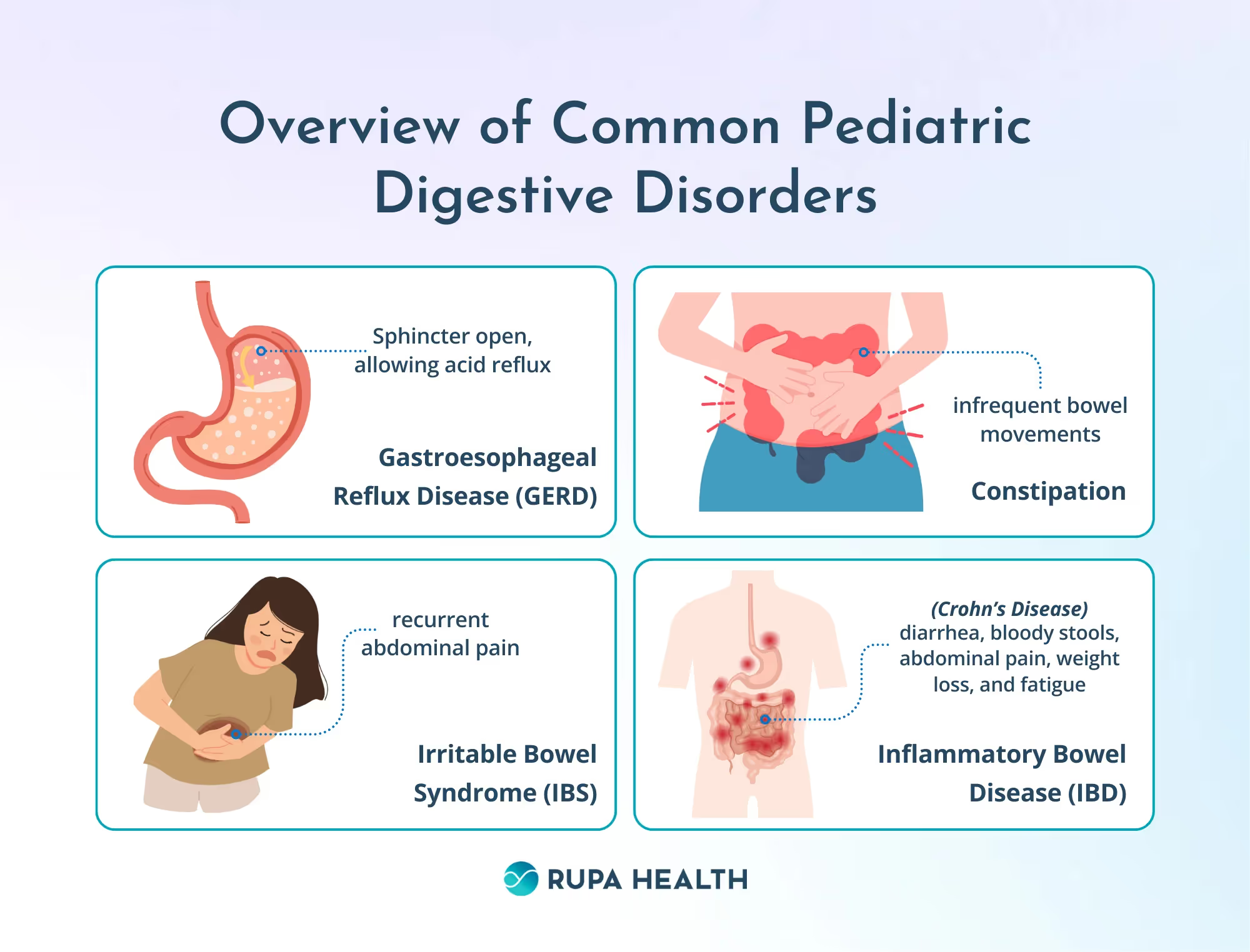
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux (GER) occurs when stomach contents backflow into the esophagus. GER is common in babies under two; most will outgrow it by 12-14 months. GERD results from chronic GER, and is characterized by troublesome symptoms and esophageal inflammation. Heartburn, described as burning chest pain, is the most common symptom of GERD. Younger children typically present with different symptoms, including cough, asthma, and trouble swallowing. Evaluation and diagnosis of GERD may include chest x-ray, upper endoscopy, barium swallow, esophageal manometry, pH monitoring, and gastric emptying studies. Treatment focuses on dietary and positional modifications, medications to reduce acid production, and calorie supplements as needed. (28, 43)
Constipation
Functional constipation affects up to 3% of children worldwide. 95% of childhood constipation is classified as functional, which is infrequent bowel movements or hard, dry stools without organic etiology. Symptoms that indicate constipation in children include infrequent bowel movements (less than three times a week), hard stools, straining, and pain with bowel movements. Diagnosis usually involves a physical exam and a detailed history. In some instances, an abdominal X-ray may be recommended to rule out fecal impaction. Treatment includes dietary changes (increased fiber and fluids), laxatives, and bowel retraining programs. (1, 18)
Irritable Bowel Syndrome (IBS)
IBS is a functional gastrointestinal disorder (FGID) that causes recurrent abdominal pain and changes to bowel habits without observable anatomical changes to the intestines. Children who have one or both parents with IBS are at highest risk for IBS. Teens are more likely to be affected by IBS than younger children. Diagnosis relies on ruling out other GI conditions and the ROME IV criteria. Treatment focuses on managing symptoms through dietary modifications, stress reduction techniques, and medication. (37)
Inflammatory Bowel Disease (IBD)
Crohn's disease and ulcerative colitis fall under the umbrella term of IBD, which causes chronic inflammation in the digestive tract. Symptoms include persistent diarrhea, bloody stools, abdominal pain, weight loss, and fatigue. IBD affects 1.6 million Americans, including 80,000 children and young adults. Very-early-onset IBD (VEO-IBD) is an IBD subtype diagnosed in children younger than six and doesn't typically respond to standard IBD treatments. Diagnosing IBD requires a colonoscopy, but the preliminary evaluation usually involves blood tests and stool analysis. Treatment aims to reduce inflammation and manage symptoms using medications, dietary changes, and, in severe cases, surgery. (36)
The Importance of Gut Health in Children
For children, a healthy gut supports their nutritional status, immune function, and mental health. A healthy gut enables efficient digestion, ensuring the smooth absorption of vitamins, minerals, and other building blocks crucial for growth and development. However, chronic GI symptoms and malabsorption disorders can disrupt this harmony, leading to feeding difficulties and risk of nutritional deficiencies. These deficiencies can have significant implications, impacting their physical growth and cognitive development, energy levels, and overall well-being.
A balanced and diverse gut microbiome – the collection of trillions of microorganisms in the intestines – supports smooth digestion, nutrient absorption, immune function, and metabolism. Alterations in this microbial ecosystem, termed dysbiosis, are linked to the development of various GI issues, including IBD, IBS, and celiac disease.
The significance of gut health in children extends beyond mere digestive capacity. Recent research has exposed the intricate relationships between the gut and the body's other systems, such as the nervous, immune, and cardiovascular systems. Studies have demonstrated intestinal dysbiotic patterns are associated with impairments in neurocognitive development, immune function, and increased risk for chronic health issues later in life. (51)
Conventional Diagnostics and Solutions for Pediatric Digestive Disorders
When a child presents with digestive trouble, the conventional approach aims to identify the specific issue and offer solutions to manage symptoms and support gut health. The diagnostic process involves obtaining a detailed medical history and physical exam to understand genetic, socioeconomic, lifestyle, and environmental factors that can contribute to symptom onset. From there, doctors will often utilize various diagnostic tests. Depending on the suspected issue, these may include blood tests to assess for inflammation, nutritional deficiencies, and food allergies; stool analysis to evaluate for blood, inflammation, and infection; and imaging to visualize internal structures. (19)
For many pediatric digestive disorders, lifestyle modifications, including dietary adjustments (i.e., fiber, hydration, and avoiding triggers), physical activity, and managing stressors, are cornerstones for conventional strategies. When these first-line approaches ineffectively manage symptoms, medications can be brought on board to address and manage symptoms. Examples of commonly prescribed medications by GI condition include:
- GERD: proton pump inhibitors, H2 blockers, and antacids
- Constipation: stool softeners, laxatives, and osmotic agents
- IBS: antidiarrheals, laxatives, antispasmodics, and antidepressants
- IBD: anti-inflammatory medications like corticosteroids and immunosuppressants
The Role of Functional Medicine Testing
While conventional medicine excels in identifying specific conditions, functional medicine delves deeper, seeking the root causes of digestive disorders in children. This personalized approach often utilizes targeted testing to assess gut health and identify imbalances. Functional medicine tests offer valuable insights beyond standard diagnostics. They enable early identification of underlying causes, individualized plans, and empowered decision-making.
Comprehensive Stool Analysis
Comprehensive stool analysis (CSA), such as the GI Effects Comprehensive Profile by Genova Diagnostics, goes beyond traditional stool tests by measuring specialty biomarkers related to intestinal digestion, absorption, and immunology, in addition to offering a detailed snapshot of the gut microbiome. Gut microbiome analysis analyzes microfloral composition and diversity and identifies pathogenic infections.
The GI-MAP is another option for mapping out the health of the gut microbiome. By providing a window into GI health and function, CSA findings point to dysbiosis, infection, inflammation, and malabsorption underlying GI function.
Adverse Food Reactions
From 1997 to 2007, the prevalence of reported food allergy increased by 18% among children under 18. Nearly 5% of children under age five have food allergies, most commonly to one or more of the following foods: milk, eggs, wheat, soy, tree nuts, peanuts, fish, and shellfish. Food allergy symptoms include vomiting, diarrhea, abdominal pain, hives, itching, and difficulty breathing. (26) Food allergies can be identified with a blood test, such as the IgE Food Allergy Advanced Test by Mosaic Diagnostics, that measures IgE immune complexes to common food proteins.
Food sensitivities are delayed immune reactions to food proteins mediated by IgG and IGA immune proteins. Symptoms of food sensitivities range from allergy-like reactions to GI symptoms to systemic symptoms like headaches, joint pain, and fatigue. Ayumetrix's Basic Food Sensitivity Panel - 96 Foods uses a blood spot sample collection – a preferred testing method for pediatric populations – to identify potential food sensitivities impacting GI health.
For children experiencing bloating, gas, and abdominal pain after consuming dairy, the Lactose Malabsorption Breath Test by Commonwealth Diagnostics International, Inc. is a non-invasive test that can help identify lactose intolerance, a non-immune mediated reaction to dairy due to a deficiency in the lactase enzyme.
SIBO Breath Test
Small intestinal bacterial overgrowth (SIBO) can mimic IBS, manifesting as bloating, pain, and altered bowel habits. A SIBO breath test, such as the SIBO - 3 Hour test by Genova Diagnostics, measures hydrogen and methane gas produced by excessive bacteria in the small intestine, leading to identification and targeted plans to support gut balance.
[signup]
Nutritional Interventions for Pediatric Digestive Disorders
When a child grapples with digestive disorders, dietary modifications become a powerful ally in managing symptoms and supporting gut health. While individual needs vary based on the diagnosis, embracing several evidence-based principles can guide a food-as-medicine approach to support.
Fiber takes center stage, with clinical trials consistently highlighting its crucial role in digestive health. Low fiber intake is associated with constipation and IBS. Higher fiber intake may improve stool consistency and frequency. Depending on the child's age and sex, children should eat 14-31 grams of fiber daily. Good sources of fiber include whole grains, legumes, whole fruits, vegetables, nuts, and seeds. (22)
Hydration is also important. When dehydrated, your digestive tract may slow down, leading to constipation, difficulty absorbing nutrients, and the potential for abdominal discomfort. Water intake may help improve IBS symptoms by supporting constipation in patients with IBS-C and preventing dehydration in patients with IBS-D.
Numerous studies highlight the link between specific foods and worsened GI symptoms in children. For example, cow's milk is a common trigger for infantile colic. In one study, a cow's milk-free diet in breastfeeding mothers resulted in colic improvements in at least one-third of infants. Up to 65% of patients with IBS report that their symptoms are related to a specific food. A detailed food-symptom diary, food sensitivity/allergy testing, and collaboration with a healthcare professional can unveil these individual triggers, paving the way for personalized dietary adjustments.
Now, let's delve into condition-specific approaches. Children with GERD may benefit from smaller, more frequent feedings to prevent overfeeding, which can exacerbate reflux. Thickening formula or breast milk with infant cereal may help reduce the frequency of acid reflux. If children have poor weight gain because of GERD, doctors may recommend a higher-calorie formula or feeding the infant through a feeding tube. (23)
Studies demonstrate the potential benefits of a low-FODMAP diet in reducing IBS symptoms. FODMAPs are short-chain carbohydrates that easily ferment and are poorly absorbed in the intestine, leading to increased gas, bowel water content, and intestinal transit. The low-FODMAP diet should be customized under the guidance of a registered dietician or other knowledgeable healthcare professional to ensure proper implementation and prevent potential caloric/nutrient deficiencies.
Chronic, intermittent elemental diet can be considered as a first-line dietary intervention for children with IBD. The elemental diet is a formula of predigested nutrients that fulfills caloric and nutritional needs. Studies show that the elemental diet may help induce remission and reduce relapse rates of IBD as effectively as corticosteroids but without their associated side effects. As an additional benefit, children eating an elemental diet may experience improved growth and development.
Herbal and Supplemental Support
While dietary modifications form the basis for managing digestive symptoms in children, incorporating safe and evidence-based herbal remedies can offer additional support.
Probiotics
Probiotics are live, beneficial microorganisms that may benefit the host when given in appropriate amounts. Probiotics can be administered to promote the abundance and diversity of desired intestinal microbes to support digestion, nutrient absorption, immune function, and intestinal integrity. Studies have shown the potential benefits of using probiotics to support constipation, diarrhea, and abdominal comfort in children. Look for age-appropriate, multi-strain probiotic supplements (containing Lactobacillus spp., Bifidobacterium spp., and/or Saccharomyces boulardii) and discuss dosage with your pediatrician, as specific strains and potencies cater to individual needs. (29)
Ginger
Because of its carminative and prokinetic properties, ginger has been used traditionally to support stomach and gastrointestinal comfort, including indigestion, gas, bloating, nausea, vomiting, and stomach pain. Ginger is recognized for its anti-inflammatory properties, suggesting a potential role in regulating inflammation in conditions such as IBD, as its bioactive constituents inhibit pro-inflammatory transcription factors. Studies have shown ginger is safe for children as young as one year. Ginger is commonly administered in whole food, tea, and capsule form.
Peppermint Oil
Given a strong level of evidence, the American College of Gastroenterology (ACG) suggests using enteric-coated peppermint oil to provide relief of global symptoms related to IBS. Peppermint contains L-menthol, which may help relax smooth muscles. Peppermint is also postulated to support GI comfort through its effects on visceral sensation and anti-inflammatory effects. (42)
In a randomized controlled trial, children with IBS were given enteric-coated peppermint oil capsules or a placebo. After two weeks, three-quarters of the patients receiving peppermint oil had reduced the severity of IBS discomfort. Enteric-coated capsules lessen the likelihood of side effects, but peppermint can induce heartburn; caution should be taken when administering to patients with GERD. (49)
Mind-Body Therapies for Digestive Symptom Relief
Mind-body therapies influence the gut-brain axis, potentially breaking the cycle that can develop between the physical and mental aspects of health. By addressing the emotional and psychological aspects alongside physical symptoms, these therapies may foster resilience in children and give them methods to manage stress and alleviate uncomfortable symptoms.
From deep breathing exercises to guided imagery, various relaxation techniques may help children manage stress and anxiety, which can trigger or worsen digestive symptoms. A 2022 study found that progressive muscle relaxation significantly reduced abdominal discomfort and improved sleep quality in children with IBS. These practices empower children to self-regulate in stressful situations.
Biofeedback uses technology to translate physiological signals, like heart rate and muscle tension, into feedback that children can use to learn to control bodily functions. By learning to modify their physiological responses, children gain valuable tools to manage discomfort independently. The results of a 2014 study suggest that heart rate variability biofeedback is a promising and effective outpatient intervention for pediatric patients with IBS and functional abdominal discomfort.
Combining physical postures, breathing exercises, and mindfulness, yoga offers a holistic approach to managing stress and digestive health. The mind-body connection cultivated through yoga empowers children to manage stress, improve flexibility, and promote relaxation. Yoga-based practices have the potential to reduce discomfort intensity, decrease school absenteeism, reduce IBS symptoms, and improve the quality of life for children with functional abdominal discomfort disorders.
Integrating Conventional and Complementary Therapies
Conventional and integrative medicine (CIM) modalities are used by 40-70% of pediatric gastroenterology patients. CIM therapies are most popular in children with low perceived effects of conventional treatment, which often occurs with FGIDs, such as IBS and functional constipation. Integrating treatments for pediatric digestive disorders can support health outcomes, reduce symptom severity, and help manage complications secondary to digestive disorders. For example, the Infectious Disease Society of America (IDSA) suggests using probiotics and zinc in children with diarrhea to support the management of diarrhea.
Assembling a team of professionals with diverse expertise optimizes care. This may include pediatricians, gastroenterologists, registered dietitians, psychologists, and complementary therapists like massage therapists or yoga instructors. Fostering open dialogue between patients, parents, and all healthcare providers to share plans, goals, and potential concerns ensures transparency and continuity of care and avoids possible conflicts.
There's no "one-size-fits-all" approach. Holistic care plans for children address each child's specific condition, triggers, and preferences. Incorporating dietary modifications, supplements, lifestyle modifications, and mindfulness practices alongside conventional therapies should be personalized based on the child's history and lab results.
[signup]
Pediatric Digestive Disorders: Key Takeaways
Embracing an integrative approach to pediatric digestive disorders holds promise for improving children's lives. By weaving conventional medicine together with evidence-based complementary therapies, we can address physical symptoms and the emotional and social aspects of these challenges. This holistic approach may help reduce discomfort, support digestion, and enhance quality of life. Open communication between healthcare providers, parents, and children is key to exploring all available options and tailoring a plan that empowers each child on their journey. A healthy gut supports a healthy child, and an integrative approach can pave the way for a brighter future.












%201.svg)






