Insulin resistance is a common metabolic dysfunction that may contribute to a number of chronic conditions such as type 2 diabetes, cardiovascular disease, and obesity. Insulin resistance occurs when cells do not respond effectively to insulin. This can lead to increased insulin production, resulting in chronically elevated insulin levels.
Much research is underway to determine the best eating patterns to help manage insulin resistance, with a low carbohydrate diet showing potential in supporting glycemic control and reducing insulin resistance. However, evidence also suggests some challenges with lower carbohydrate diets.
[signup]
The Role of Insulin in the Body
Insulin is a hormone released by pancreatic beta cells when blood glucose rises. When carbohydrates are ingested and metabolized, blood glucose rises, signaling the body to release insulin. Insulin functions in two main ways: to help manage blood glucose levels and to act as a signaling molecule for various cells.
Insulin resistance indicates a metabolic disruption occurring when cells do not respond effectively to insulin. In turn, the pancreas releases more insulin to overcome this blunted response. Eventually, blood glucose can remain consistently elevated, which may contribute to type 2 diabetes mellitus. A chronically elevated insulin level may perpetuate inflammation, which can worsen chronic disease progression.
Factors Contributing to Insulin Resistance
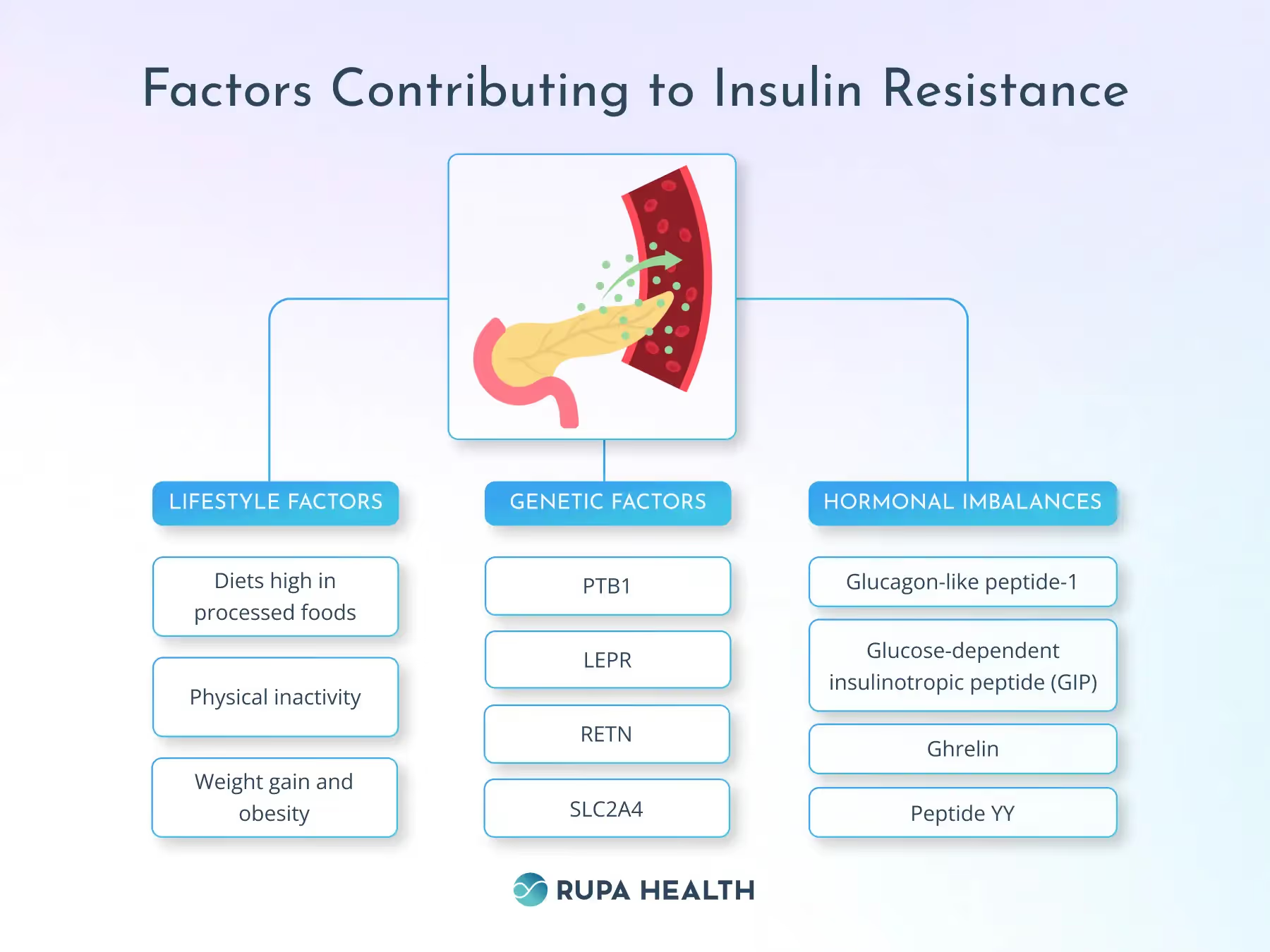
Lifestyle Factors
- Diets high in processed foods, including added sugars, refined carbohydrates, and processed meats, may cause the pancreas to release more insulin, potentially resulting in a proinflammatory state and increasing the risk of insulin resistance.
- Physical inactivity is a risk factor for developing insulin resistance.
- Weight gain and obesity are independent risk factors for insulin resistance.
Genetic Factors
Genetic predispositions, such as variations in genes coding for insulin signaling or genetic factors affecting mitochondrial activity, lipid metabolism, and inflammatory mediators, can also increase the risk of insulin resistance.
Examples of genetic markers that may increase the risk for insulin resistance include these:
- PTB1
- LEPR
- RETN
- SLC2A4
Hormonal Imbalances
Imbalances of neuroendocrine hormones may directly affect insulin levels, including the following:
- Glucagon-like peptide-1
- Glucose-dependent insulinotropic peptide (GIP)
- Ghrelin
- Peptide YY
Conditions like polycystic ovarian syndrome (PCOS) and metabolic syndrome are associated with elevated insulin levels and reduced insulin activity, which may increase the risk of weight gain and type 2 diabetes mellitus.
Low Carbohydrate Diets and Insulin Resistance
Low carbohydrate diets limit the intake of carbohydrates and in their place, emphasize protein and fat. They vary depending on the amount of carbohydrates they recommend.
- Low carbohydrate diets: < 40% of calories from carbohydrates, 25-30% of calories from protein, and 30-40% of calories from fat
- Ketogenic diets (more extreme version, designed to induce ketosis): 5-10% of calories from carbohydrates, 20-30% of calories from protein, and 60-75% of calories from fat
Potential Benefits for Insulin Sensitivity
Low carbohydrate diets have been shown to support insulin sensitivity, especially in individuals who are overweight or obese. Reducing carbohydrate intake may help manage blood sugar levels, thus decreasing insulin secretion. As insulin levels are lower, insulin sensitivity can improve.
The added benefit of weight loss from low carbohydrate diets may also enhance sensitivity to insulin. With improved insulin sensitivity, low carbohydrate diets can be effective in helping manage type 2 diabetes mellitus. Very low carbohydrate diets (as with the ketogenic diet) present sustainability concerns in the long term, so finding the proper balance of macronutrients through a personalized nutrition plan may help optimize outcomes.
Risks and Considerations
While low carbohydrate diets offer many potential benefits, they also have risks and potential negative side effects.
- Nutrient deficiencies can occur, including fiber, vitamins, and minerals.
- Elevated cholesterol levels are possible with increased consumption of saturated fats.
- Healthy individuals may have paradoxical reactions to ketogenic diets, potentially affecting insulin sensitivity and glucose metabolism.
- Long-term adherence may be difficult, limiting food options.
Balancing Carbohydrate Intake
A moderate carbohydrate intake, including 45-55% of total daily calories from carbohydrates, offers a more balanced diet approach that may support insulin sensitivity across various populations. Potential benefits of a moderate carbohydrate diet include:
- Allows for sufficient carbohydrate consumption for energy
- May help maintain insulin sensitivity
- Evades the extremes of low-carbohydrate diets
- Weight loss while maintaining muscle mass
- More sustainable long-term
For individuals with varying metabolic profiles, including conditions of overweight, obesity, and insulin resistance, moderate carbohydrate intake can help stabilize blood sugar levels and support insulin sensitivity without risking nutrient deficiencies or other negative side effects. Its long-term sustainability makes it a comfortable plan for many people.
Implementing a Low Carbohydrate Diet Safely
While controlling carbohydrate intake may help reduce insulin resistance, personalizing dietary approaches is necessary for optimal management. Variables such as other health conditions, metabolic biomarkers, preferences, and other lifestyle factors should be considered. Individual response to different diets varies, warranting tailored approaches. It is important to establish a plan that is sustainable and incorporates desirable foods for long-term adherence.
Monitoring and Adjusting Your Diet
Implementing a low carbohydrate diet should be done under the supervision of a healthcare professional, who can make individualized recommendations. Regularly monitoring biomarkers of blood glucose, hemoglobin A1c, cholesterol levels, and weight is necessary to track progress and monitor for adverse effects like ketonuria. Continually adjusting personalized carbohydrate recommendations based on health goals and progress. Ensuring nutrient density within vegetables, lean proteins, and healthy fats will help meet essential nutrient needs. Adequate water intake will help support digestion, promote fullness, and promote overall health.
Alternative Strategies for Managing Insulin Resistance
Beyond Diet: The Role of Physical Activity
Regular physical activity is important to support insulin sensitivity. Cardiovascular exercise may increase glucose uptake and utilization in muscles. It also helps promote a healthy weight by increasing energy expenditure and promoting fat oxidation. Strength training may improve insulin sensitivity by increasing muscle mass and glucose uptake into muscles. Strength training helps increase and preserve lean body mass, supporting long-term weight management by increasing resting energy expenditure.
Lifestyle Changes
Early identification of insulin resistance is important for delaying or managing the onset of type 2 diabetes, cardiovascular disease, and other associated metabolic conditions. It allows for management with lifestyle interventions first.
In addition to proper nutrition and physical activity, managing insulin resistance may require stress management and adequate sleep. Using personalized approaches may provide effective patient-centered care to support overall health outcomes.
[signup]
Key Points
- Insulin resistance is a multifaceted, proinflammatory condition that may predispose individuals to metabolic syndrome, type 2 diabetes, cardiovascular disease, and obesity.
- Dietary modifications may help manage insulin resistance by supporting glycemic control and a healthy weight.
- Controlled carbohydrate diets may reduce the risk of insulin resistance or help manage its progression.
- Focusing on personalized nutrition guidelines and a healthy lifestyle may help promote optimal health and well-being.












%201.svg)









.png)
