In the United States, M.D. (Doctor of Medicine) is traditionally seen as the standard title for physicians. However, an increasing number of practitioners hold the D.O. (Doctor of Osteopathic Medicine) credential. Like M.D.s, D.O.s are fully licensed to practice medicine and share similar rights and responsibilities. Still, their training also integrates osteopathic principles, which emphasize a holistic approach to patient care.
This article explores the similarities and differences between these two physician pathways and examines how they can shape a patient’s overall healthcare experience.
[signup]
What is an M.D.?
An M.D. (Doctor of Medicine) is a fully trained physician who diagnoses, treats, and helps prevent illnesses and injuries through evidence-based, allopathic medical practices.
To become an M.D., students first earn a bachelor’s degree (often in a pre-medical or science-focused track). They then apply to a four-year [LCME]-accredited medical school program and begin their formal training as doctors.
In a traditional medical school, students learn allopathic medicine, which includes evidence-based diagnostics and treatments such as surgery, pharmaceuticals, and other conventional medical interventions. In addition to focusing on specific symptoms, M.D.s also receive training in preventive care, although emphasis may vary among programs and individual physicians.
What is a D.O.?
Doctors of Osteopathy (D.O.s) also complete a bachelor’s degree and then attend medical school. During osteopathic medical training, students focus on the musculoskeletal system, including osteopathic manipulative treatment (OMT)
D.O. curricula often place additional emphasis on communication skills and lifestyle factors influencing health.
Students choosing the D.O. path have steadily increased in the last few years. According to the American Association of Colleges of Osteopathic Medicine (AACOM), the number of American osteopathic doctors has increased by 64% since 2013, with new osteopathic medical schools opening and existing programs expanding throughout the country.
While many D.O.s choose primary or family medicine, they can also pursue any specialty or subspecialty, similar to M.D.s.
D.O. and M.D. Licensing
After graduating from an accredited medical school, physicians must complete a residency (of three to seven years) before they can practice independently. During that time, a new doctor receives hands-on experience working with patients. These programs are accredited by the Accreditation Council for Graduate Medical Education (ACGME) to ensure quality and consistency of training.
Both M.D.s and D.O.s must complete residency programs in order to gain practical experience under the supervision of senior physicians.
M.D.s must pass all three parts of the United States Medical Licensing Examination (USMLE) to obtain a medical license. D.O.s take an equivalent exam called the Comprehensive Osteopathic Medical Licensing Examination (COMLEX).
Once M.D.s and D.O.s are fully licensed to practice medicine, they can prescribe medications, diagnose and treat diseases, and perform procedures and surgeries. Often, doctors will continue to get board certified, which is an advanced certification given by a board of experts in the physician’s chosen area of specialty.
Key Differences Between D.O.s and M.D.s
While the guiding philosophies differ, in practice there can be significant overlap in how individual M.D.s and D.O.s care for patients. (Table 1).
A D.O. might place additional emphasis on dietary, exercise, and psychosocial factors before or alongside medication management. Many M.D.s also address these factors but may emphasize pharmacological treatment earlier, depending on the individual physician’s approach and the patient’s needs.
Table 1: Similarities and differences between allopathic and osteopathic medicine.
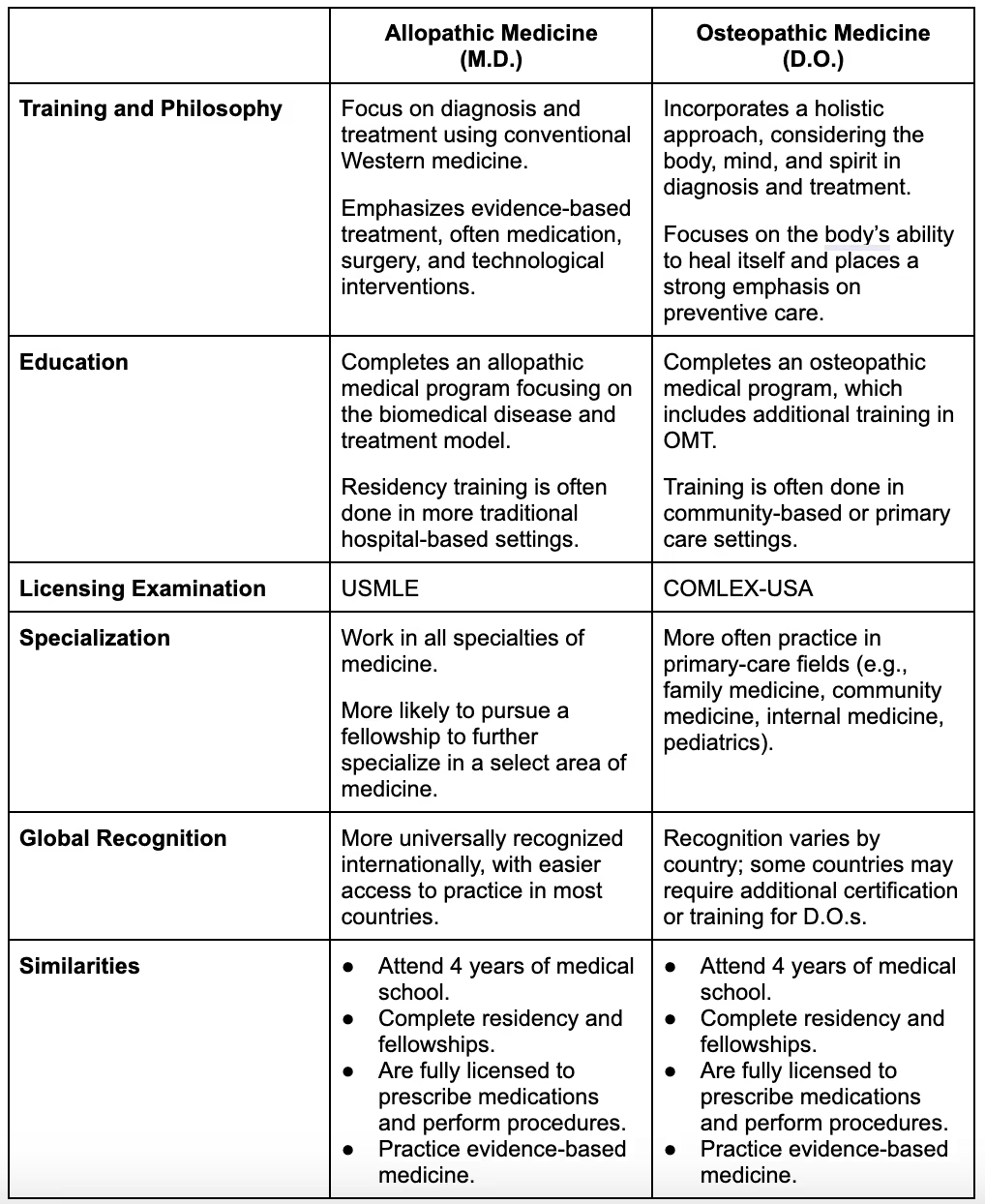
Note: Individual physician practices may vary.
Patient Perspective: Choosing Between an M.D. and a D.O.
There are a few specific concepts to consider before choosing a practitioner:
D.O.s often focus on disease prevention through lifestyle, exercise, and diet modifications, while many M.D.s also address prevention but may place different emphasis on medication and technology-based treatments.
All patients carry significant responsibility in following medical advice. However, a D.O. might spend more time on preventive strategies and lifestyle interventions, while an M.D. might focus more on pharmacologic interventions early on, depending on the clinical scenario.
Frequently Asked Questions
Q: Can a D.O. perform surgery?
A: Yes. D.O.s can perform the same surgeries as M.D.s provided they have completed the requisite surgical training and board certifications.
Q: Is one pathway more rigorous than the other?
A: No. Both have similarly stringent academic and clinical requirements, although the emphasis and specific curricula differ.
Q: How can I find a D.O. in my area?
A: You can search by zip code on the American Osteopathic Association’s online “Find a D.O.” directory.
[signup]
Key Takeaways
- Both M.D.s and D.O.s are trained and licensed medical professionals.
- Both can diagnose, treat, prescribe medications, and perform surgery.
- D.O.s often emphasize whole-person approaches, while M.D.s often emphasize allopathic treatment—but many physicians in both pathways practice a blend of these approaches.












%201.svg)







