Hearing about a "brain-eating amoeba" can sound scary. This microscopic organism, called Naegleria fowleri, is naturally found in warm freshwater like lakes, rivers, and hot springs. In rare cases, it can infect humans when contaminated water enters the nose, travels to the brain, and causes a severe infection.
While cases are extremely rare, they are often serious. This article explores the symptoms of Naegleria fowleri infection, available treatments, and practical prevention tips.
[signup]
What is a Brain-Eating Amoeba?
The term “brain-eating amoeba” refers to Naegleria fowleri, a tiny organism that lives in warm freshwater. It is called an amoeba because it belongs to a group of single-celled organisms that move and feed by changing shape. While Naegleria fowleri usually feeds on bacteria, it can sometimes enter the human body and cause a serious infection.
Definition and Explanation
Naegleria fowleri is a free-living amoeba, meaning it doesn’t rely on a host to survive. It thrives in warm environments, especially in freshwater lakes, rivers, hot springs, and poorly maintained pools or water systems. It is not found in saltwater like oceans.
This amoeba causes primary amebic meningoencephalitis (PAM), a rare but often fatal brain infection. It’s important to note that this infection is rare, with only a few cases reported yearly.
Scientific Classification
Naegleria fowleri belongs to the Naegleria genus, which includes several species, but only fowleri is known to infect humans. It is classified as a "thermophilic" amoeba, meaning it thrives in warm temperatures, typically between 77°F and 115°F (25°C to 46°C).
Lifecycle and Transmission
The lifecycle of Naegleria fowleri includes three stages:
- Cyst – A dormant, protective stage when conditions are not favorable.
- Trophozoite – The active feeding stage that can cause infection.
- Flagellate – A temporary swimming stage.
The infection occurs when contaminated water enters the nose. From there, the trophozoites travel up the olfactory nerve, which connects the nose to the brain. Once in the brain, the amoeba begins feeding on brain tissue, leading to inflammation and severe symptoms.
The infection cannot spread from person to person or by drinking contaminated water. It only occurs when water with the amoeba directly enters the nasal passages. Understanding this helps in taking preventive measures when swimming or using warm freshwater.
Symptoms and Diagnosis
Recognizing the symptoms of a Naegleria fowleri infection is critical, as early detection offers the best chance for effective treatment. However, because the infection is so rare and symptoms resemble other illnesses, it can be challenging to identify.
Early Symptoms of Infection
The infection starts with symptoms that are easy to confuse with bacterial or viral meningitis. These early signs typically appear 1–12 days after exposure and may include:
- Severe headaches
- Fever
- Nausea and vomiting
- Stiff neck
Since these symptoms overlap with common illnesses, early detection is often delayed. However, prompt medical attention during this stage is vital.
Progression of Symptoms
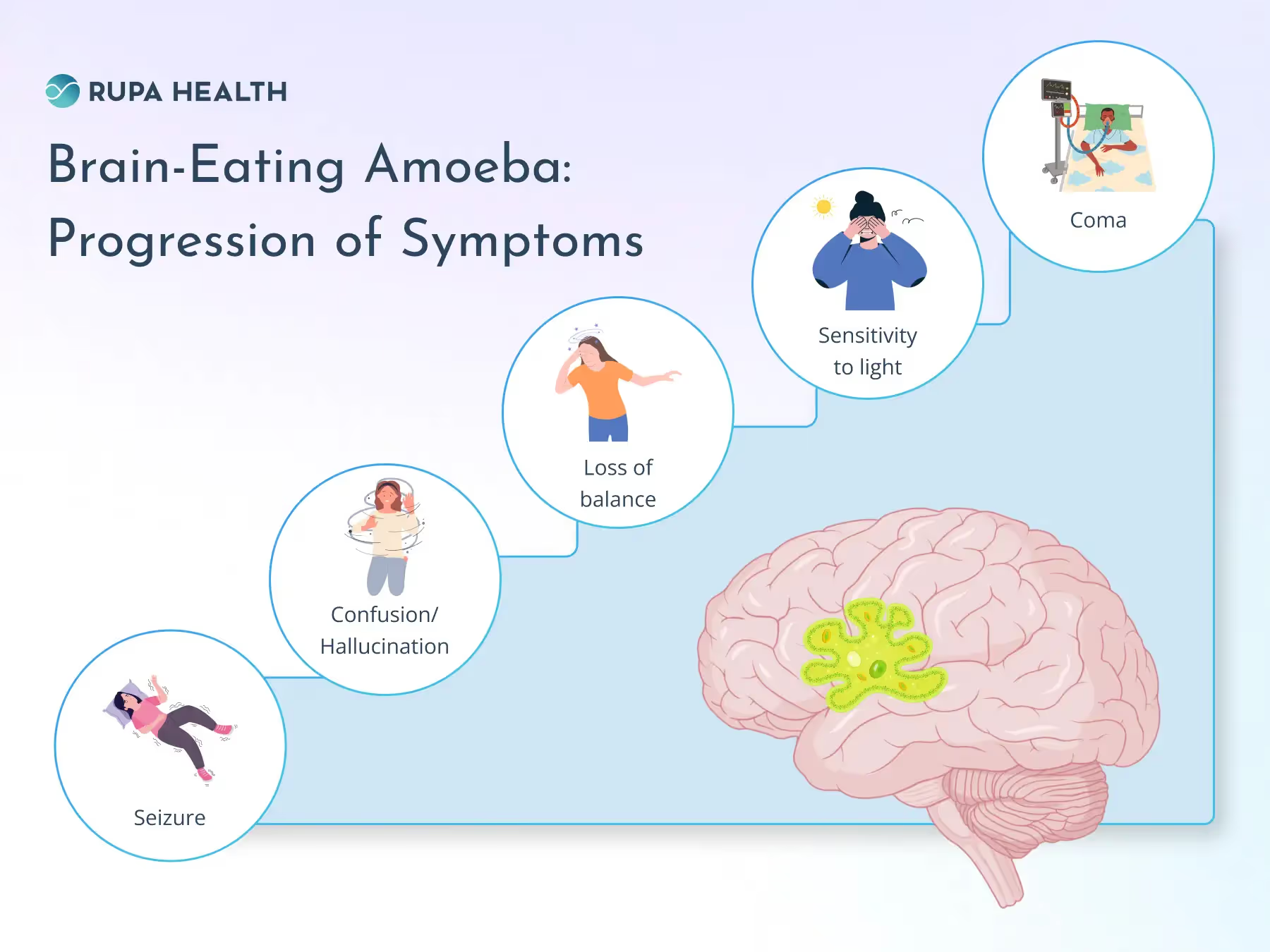
If untreated, the infection can progress rapidly, sometimes within days, leading to severe and life-threatening symptoms such as:
- Seizures
- Confusion or hallucinations
- Loss of balance
- Sensitivity to light
- Coma
The disease progresses quickly, so acting on the first signs of trouble can make a big difference.
Diagnostic Methods
Doctors use several tools to confirm a Naegleria fowleri infection, including:
- Spinal Tap (Lumbar Puncture): This test collects cerebrospinal fluid to check for signs of infection or detect the presence of the amoeba.
- Imaging Tests: Brain MRI or CT scans can help identify swelling or damage in the brain.
- PCR Tests: Polymerase chain reaction tests are highly specific and can detect the DNA of Naegleria fowleri.
- Microscopic Examination: Fluid samples may also be examined under a microscope to look for the amoeba.
Diagnostic Challenges
Because Naegleria fowleri infections are so rare, they are often misdiagnosed or diagnosed too late. The symptoms mimic other conditions like bacterial meningitis, leading to delays in proper treatment. Additionally, many healthcare providers may not consider this infection due to its rarity. Increased awareness and faster diagnostic tools are crucial for improving outcomes.
Treatment Options
Treating a Naegleria fowleri infection is challenging, as the disease progresses rapidly and often isn’t detected until it’s advanced. While some treatments have shown promise, success largely depends on early diagnosis and swift intervention.
Current Treatments
Doctors use a combination of medications to treat the infection, focusing on antifungal and antimicrobial drugs that may help stop the amoeba’s spread. Key treatments include:
- Miltefosine: Originally developed to treat certain parasitic infections, miltefosine has been used in combination with other therapies for Naegleria fowleri. It works by targeting the amoeba’s cell membrane.
- Amphotericin B: This powerful antifungal medication is administered intravenously and directly into the brain in some cases. It helps kill the amoeba but can have severe side effects.
In addition, therapeutic hypothermia is sometimes used. This involves cooling the body to reduce brain inflammation and limit damage. It has been used successfully in a few cases when combined with medications.
Experimental Therapies
Because Naegleria fowleri infections are so rare, research into new treatments is ongoing. Experimental approaches include:
- Improved Drug Formulations: Efforts to develop medications that target the amoeba more effectively with fewer side effects.
- Immune-Based Therapies: Treatments that enhance the body’s ability to fight the infection.
- Clinical Trials: Ongoing studies aim to identify new drugs or combinations that may improve survival rates.
While these approaches are promising, they are still in the experimental stages and not widely available.
Challenges in Treatment
One of the biggest hurdles in treating Naegleria fowleri infections is the fast progress of the disease. The amoeba causes significant brain damage in just days, and symptoms often resemble more common illnesses, delaying diagnosis. Most patients are diagnosed only after the infection has advanced, limiting treatment options.
Prevention Strategies
Reducing the risk of Naegleria fowleri infection involves both personal precautions and public health efforts. While the infection is rare, limiting exposure to contaminated water can help prevent it.
Personal Prevention
One of the simplest ways to lower risk is by avoiding swimming or diving in warm freshwater lakes, rivers, or hot springs, especially during the summer when water temperatures are higher.
- If swimming in these waters is unavoidable, using a nose clip can help block water from entering the nasal passages, the primary route for the amoeba to reach the brain.
- Avoiding activities like diving or jumping into warm freshwater, which forces water up the nose, can reduce exposure.
Environmental Controls
Public health measures also play a role in prevention. For example, water treatment protocols can help keep recreational water sources safer. This may involve chlorination or other disinfection techniques in public pools or water parks.
Local authorities can also monitor high-risk water bodies for the presence of Naegleria fowleri and issue advisories when necessary.
Awareness and Education
Education is a critical tool in preventing infections. Communities in regions with warm freshwater should be informed about the risks of Naegleria fowleri and the steps to take to protect themselves. Public health campaigns, school programs, and community workshops can raise awareness and teach individuals how to enjoy natural water sources safely.
Brain-Eating Amoeba: Global Incidence and Risk Factors
While Naegleria fowleri infections are rare, certain geographical and environmental conditions make some regions and populations more vulnerable. Understanding where and when this amoeba will likely thrive helps identify and manage the risks.
Geographical Distribution
Naegleria fowleri is most commonly found in warm freshwater environments worldwide. Areas with higher incidence rates include the southern United States, particularly states like Texas and Florida, and parts of Asia, Africa, and Australia.
The amoeba thrives in warm climates, and infections are typically reported in regions where water temperatures exceed 77°F (25°C). Cases have also been linked to untreated or poorly maintained water systems, such as swimming pools or tap water used for nasal rinsing.
Seasonal and Environmental Risk Factors
Infections are most common during the summer months, when water temperatures are higher, and people are more likely to engage in recreational water activities. Climate change may also increase the frequency of cases as rising global temperatures expand the habitable range for Naegleria fowleri.
Prolonged heat waves and droughts can create ideal conditions for the amoeba to thrive in stagnant, warm water.
At-Risk Populations
Certain groups are more likely to be affected by Naegleria fowleri. Children and young adults are at greater risk because they tend to participate in water activities that increase the chance of water entering the nose, such as swimming, diving, or splashing. Outdoor swimmers in warm freshwater during the summer face the highest risk.
The Role of Healthcare Professionals
Healthcare professionals are crucial in identifying, managing, and preventing Naegleria fowleri infections. Their actions can significantly impact the outcomes for affected patients and help reduce risks for communities.
Importance of Early Detection
Healthcare providers are on the front line of recognizing the symptoms and risk factors of Naegleria fowleri. Early symptoms, such as severe headache, fever, nausea, and stiff neck, can mimic other conditions like bacterial meningitis.
Awareness of exposure to warm freshwater or high-risk activities, such as swimming in untreated water, can prompt doctors to consider this rare infection possible. Using advanced diagnostic tools like PCR testing or imaging scans early in the diagnostic process can help confirm the presence of the amoeba before the infection progresses.
Communication with Patients
Patient education is a critical responsibility for healthcare professionals. When discussing risks, it’s important to provide clear and simple information. For instance, explaining how warm freshwater environments and nasal exposure increase the likelihood of infection can help individuals take preventive measures.
Additionally, community education efforts, including talks, posters, and digital resources, can raise awareness in high-risk areas. Establishing trust and encouraging patients to report unusual symptoms promptly can also lead to earlier diagnosis and treatment.
Research and Advocacy
Healthcare professionals contribute to ongoing research aimed at improving diagnostic techniques, developing more effective treatments, and understanding the spread of Naegleria fowleri.
Advocacy for funding and awareness is also key to advancing scientific efforts. By staying informed about emerging therapies and participating in clinical trials or case studies, providers can play a role in improving outcomes and expanding the knowledge base for this rare condition.
[signup]
Key Takeaways
- Naegleria fowleri, or "brain-eating amoeba," is a rare but often fatal organism found in warm freshwater. When contaminated water enters the nose, it can cause primary amebic meningoencephalitis (PAM).
- Early symptoms like headache, fever, nausea, and stiff neck can mimic meningitis, making diagnosis challenging, while advanced stages involve seizures, confusion, and coma.
- Treatment involves antifungal and antimicrobial drugs like amphotericin B and miltefosine, often combined with therapeutic hypothermia, though early diagnosis is critical for survival.
- Preventive measures include avoiding warm freshwater activities, especially in summer, using nose clips, and ensuring proper disinfection of pools and water systems.
- Raising awareness in at-risk areas, improving diagnostic tools, and developing effective treatments through research are vital steps in managing and reducing infections.












%201.svg)








.png)
