Neurodegenerative diseases are often considered to be a normal part of aging, and with Alzheimer’s disease being the third leading cause of death for Americans in 2019, it would make sense. Despite the billions of dollars that are spent on Alzheimer’s research each year, we seem to be no closer to a cure. This could be related, in part, to how we traditionally think about treating brain health diseases. Overall, our efforts have been to identify and treat one cause of neurodegeneration, but the truth is many different factors impact brain function in an individual.
So, what's the answer? Protecting your brain and preserving excellent brain function throughout your life requires a personalized treatment approach. Reversing the poor brain health that plagues so many requires us to move toward the integrative management of neurodegenerative diseases. This model tailors traditional and alternative therapies to a specific person, which allows for better quality of life and disease outcomes.
[signup]
What Are Neurodegenerative Diseases?
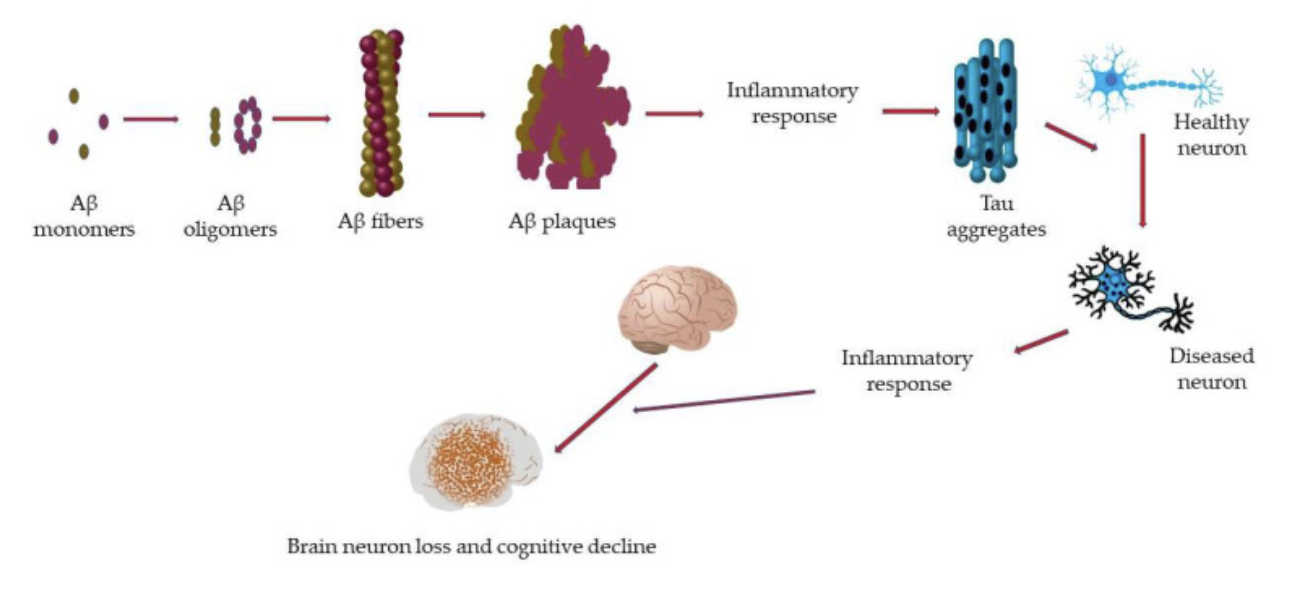
Neurons (nerve cells) are the workhorses of the brain and nervous system. They can be created throughout life, but their numbers decline during aging. This loss of neurons, combined with damage to their structure and function, defines neurodegeneration. When neurons are lost, damaged, and/or not functioning optimally, communication and neural networks are disrupted, and protein variants (like tau proteins) are deposited in the brain. Here’s an image depicting the overview of neurodegenerative diseases and the process that leads to cognitive decline:
Neurons assist with everything from thinking, feeling pain or pleasure, and emotions to breathing, digestion, and sleeping. It’s thought that genetics and environmental factors (like insulin resistance, gut dysbiosis, an inflammatory diet, toxin exposure, and stress) contribute equally to the loss and damage of neurons and, ultimately, disease development. Since neurons are intimately tied to all bodily functions, people with these conditions may have difficulty with tasks we take for granted, like speaking, walking, bowel and bladder functions, and recalling information.
The most well-known neurodegenerative diseases are Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS), but Huntington’s disease, spinal muscular atrophy, and spinocerebellar ataxia also fit into this category.
What is Alzheimer’s Disease?
Alzheimer's Disease (AD) is the most common type of dementia, typically affecting people over the age of 65. It’s characterized by the accumulation of neurofibrillary tangles and beta-amyloid plaques in the brain, although these may be a consequence of the neurodegenerative process rather than the cause. Plaque impacts the function of the hippocampus, and patients can have extensive loss of nerve cells, disrupted synapses, and altered neurotransmitter function. As a result, people with AD begin to have difficulty recalling information, and they progressively decline, experiencing errors in judgment, thinking, and speaking.
What is Parkinson’s Disease?
Parkinson's Disease (PD) is a progressive neurodegenerative disease characterized by tremors, difficulty with balance, coordination, and walking, and muscle stiffness. Dysfunction occurs with α-synuclein, a protein involved in synapse trafficking and neurotransmitter release. But mitochondrial dysfunction, the inability to clear proteins from the brain, and neuroinflammation are also key features. PD is characterized by atrophy of the frontal cortex, death of dopaminergic neurons, and enlargement of brain ventricles, which damages brain tissue. Lewy bodies and neurites, as well as beta-amyloid plaques, can be present.
What is Amyotrophic Lateral Sclerosis (ALS)?
Amyotrophic Lateral Sclerosis (ALS) progressively damages the nerve cells and spinal cord, resulting in muscle weakness and paralysis, and patients often pass away from respiratory failure 3-5 years after symptom onset. While there are many genes associated with ALS, four main genes are responsible for more than 70% of ALS cases (C9orf72, TARDBP, SOD1, and FUS). Dysfunction in DNA repair, mitochondrial function, and glial cell function contribute to motor neuron decline, which leads to the degenerative process. Patients with ALS also have protein aggregation between neurons, most commonly the TAR DNA binding protein.
Functional Medicine Lab Testing for Neurodegenerative Disease Management
Conventional tests like hs-CRP, homocysteine, a thyroid panel, and HbA1c can provide some insight into the root causes of brain health symptoms like inflammation, hyperglycemia, and altered thyroid hormone levels, which makes it easier to design an effective treatment plan. Functional medicine testing for neurodegenerative diseases takes it a step further and looks for root causes that may be overlooked. Personalizing treatment with lab tests is an important way to optimize outcomes. Here are some tests to consider:
Comprehensive Stool Testing
Poor gut health may contribute to neurodegenerative diseases. The GI-MAP stool test from Diagnostic Solutions detects microbial imbalances and potentially pathogenic microbes but also gives insight into digestion, absorption, inflammation, and immune system function.
Diabetes Testing
Insulin resistance and hyperglycemia can lead to chronic inflammation, which is a root cause of poor brain health. Measuring biomarkers associated with the diagnosis of diabetes, like fasting insulin, fasting glucose, and hemoglobin A1c can be used to give a more complete picture of blood sugar regulation.
Micronutrient Testing
Neurons require massive amounts of ATP, and the creation of ATP requires nutrients. The Spectracell Micronutrient Test analyzes various vitamins, minerals, and other nutrients to determine if poor nutrient status is underlying brain health symptoms. Practitioners can tailor the meal plan or supplement recommendations to optimize nutrient intake.
Neurotransmitter Testing
The NeuroBasic profile from Doctor’s Data can provide an assessment of nervous system health. This urine-based test provides various neurotransmitter levels to clue practitioners into possible imbalances.
[signup]
Conventional Treatments and Their Limitations
Current traditional treatments for neurodegenerative diseases aim to improve disease symptoms, but some attempt to target the underlying disease process to prevent or delay progression.
Approved treatments for AD include drugs to target and remove beta-amyloid plaques, cholinesterase inhibitors to preserve acetylcholine (an essential neurotransmitter for memory and muscle contraction), and glutamate regulators (glutamate is an excitatory neurotransmitter for learning and memory). Unfortunately, none of these offers any real solution or improvement for AD patients. For example, Aducanumab (an IV infusion to target beta-amyloid plaques) does reduce beta-amyloid, but this hasn’t translated into improved cognitive function in AD patients. And cholinesterase inhibitors and glutamate regulators only improve cognitive function slightly without any meaningful delay in disease progression.
Likewise, there are currently no treatments that target the underlying causes of PD. The approved pharmaceuticals are used mainly to alleviate motor and other PD symptoms by replenishing dopamine levels. These drugs include dopamine supplements, decarboxylase inhibitors to reduce the breakdown of levodopa, and dopamine agonists to provide dopamine effects.
Patients with ALS are often treated with free radical scavengers and glutamate receptor antagonists, which inhibit glutamate receptors. Medications for ALS patients may delay death by 3-4 months and slow disease progression to a certain extent, but there are currently no treatments that reverse the disease process.
As you can see, there are significant limitations of conventional therapies. For example, unlike simple illnesses like pneumonia, where there’s one target, neurodegenerative diseases have many contributors, so there are many targets to consider. This makes it practically impossible for one medication to provide a meaningful impact for such complex conditions. In addition, the blood-brain barrier (BBB) creates a unique challenge when attempting to deliver therapeutic doses of medication into the brain.
While medications may help to improve symptoms for some, the outcome for all of these neurodegenerative diseases is quite bleak. However, an integrative approach that considers all the contributing variables in a specific person may be efficient for disease prevention, delay, or even reversal.
Dietary Interventions for Neurodegenerative Disease Management
Nutrients are required for every process that occurs in the body, and the brain is no exception. The brain uses energy in the form of adenosine triphosphate (ATP), and the creation of ATP requires nutrients. If nutrients are in short supply, the brain ends up with less energy. Still, it’s also unable to protect itself from inflammation, insulin resistance, oxidative stress, free radicals, and toxins - all possible contributors to nerve cell dysfunction and death. Optimizing nutrient status through diet may be one way to preserve nerve cells and their function.
There is a spectrum of brain-healthy dietary patterns to choose from. The Mediterranean diet, the MIND diet, and the KetoFLEX 12/3 plans are all evidence-based options.
The Mediterranean Diet for Neurodegenerative Disease Management
The Mediterranean diet focuses on antioxidant-rich fruits and vegetables, flavorful herbs, legumes, beans, minimally processed whole grains, healthy fats, nuts, and seeds. This eating style can target inflammation and improve gut health and is associated with better cognitive function.
The Mediterranean-Dietary Approaches to Stop Hypertension Intervention for Neurodegenerative Delay (MIND) Diet
The MIND diet combines the Mediterranean and DASH diets in an attempt to specifically target brain health. This meal pattern has also been associated with better cognitive function and a lower risk of dementia. It’s similar to the Mediterranean diet but emphasizes green leafy vegetables and berries.
KetoFLEX 12/3 Diet
The KetoFLEX 12/3 meal plan focuses on plant-based foods that are nutrient-dense. Care is taken to emphasize organic options, seasonal non-starchy vegetables, lean protein, healthy fat, and fasting. The KetoFLEX 12/3 diet, as part of a personalized treatment plan, may improve cognition in people with mild cognitive impairment (MCI).
Most research studies on dietary treatments are observational in nature, so it’s difficult to know what specific components of a diet lead to the improvement. Likely, it’s the dietary pattern rather than its individual components that provide the benefits. What we do know is that wholesome food has the ability to target and mitigate the common underlying causes of disease in the body.
Nutritional Supplementation
In addition to a personalized, nutrient-dense diet that’s very low in simple sugars, inflammatory fats, and ultra-processed foods, nutritional supplements for neurodegenerative diseases can be essential. Here are some nutritional supplement options for brain health.
Choline
Choline is an important nutrient that’s made in small amounts in the human body, and low levels have been associated with poor cognitive function. Choline acts as a methyl donor to aid in creating phospholipids, which are needed for brain cell membrane structure and communication. It’s also a precursor to acetylcholine, which is important for memory. Foods with the highest amounts of choline are animal-based, so people who follow a primarily plant-based diet may need to supplement. The adequate intake (AI) for choline is 550 mg/day and 425 mg/day for men and women respectively.
B Vitamins
The B vitamins are integral for proper brain function since they act as coenzymes for the creation of energy, help with DNA and RNA creation and repair, assist with methylation and help to create neurotransmitters and other brain cell communication molecules. Research suggests multivitamins that include B vitamins may help to improve cognition and memory.
Vitamin D
Vitamin D aids in brain cell communication, increases synaptic plasticity and may help the immune system remove beta-amyloid plaques from the brain. Low vitamin D levels are associated with cognitive decline. The sun is the primary source of vitamin D, so people who live in areas where sunlight is limited or those who spend the majority of their time indoors are at risk for inadequate vitamin D levels. It’s important to have vitamin D levels checked and then personalize supplementation.
Omega-3 Fatty Acids
Omega-3 fatty acids are important for nerve cell membrane structure and function, but they also help to form communication molecules. Low omega-3 levels and/or an imbalanced omega-6 to omega-3 fatty acid ratio are associated with poor cognitive function and a higher risk of dementia. One omega-3, docosahexaenoic acid (DHA), helps to lower inflammation, increase brain-derived neurotrophic factor (BDNF - a protein important for brain cell growth and survival), and reduce oxidative stress.
The AI for omega-3s is 1.6 grams/day for men and 1.1 grams/day for women. The best food sources are seafood-based, so if you don’t eat fish often, or if you have an allergy to fish, you may be lacking in omega-3s. Supplements can be a great option, and in the case of allergy, algae oil is an excellent source of omega-3s.
Probiotics
Probiotics can rebalance the gut microbiome, lower inflammation, and increase BDNF, all of which are important for those with neurodegenerative diseases. One meta-analysis found probiotics to improve cognitive function, memory, and the ability to perform daily activities in people with AD.
Physical Activity and Neurodegenerative Diseases
Humans are meant to be physically active, so exercise may be one of the most vital strategies for maintaining excellent brain health throughout the lifespan. Research has confirmed that sedentary people have almost two times the risk of developing cognitive decline when compared to those who are physically active.
Exercise benefits in neurodegenerative diseases include physically increasing blood flow and thus nutrients and oxygen to the brain and its cells, promoting the production of BDNF, promoting neuroplasticity to form new neural connections, stimulating the release of neurotransmitters, and supporting recovery after a brain injury. Exercise also combats many of the root causes of neurodegeneration, like obesity, insulin resistance, inflammation, stress, and high blood pressure.
Exercise is excellent for disease prevention, but it’s also a valuable tool for those who already have a neurodegenerative condition. Both aerobic activity and strength training have been shown in meta-analyses to improve brain function. When exercise was compared to donepezil (Aricept) in patients with mild cognitive impairment (MCI) and those with AD, exercise led to improved cognitive function and was superior to the drug. Both aerobic and resistance training led to significant increases in BDNF in those with neurodegenerative diseases like MCI, AD, and PD.
Incorporating physical activity for brain health can be as simple as starting with a 10-minute walk after meals and then progressively increasing to the recommended 150 minutes of moderate-intensity or 75 minutes of vigorously intense aerobic exercise (running, brisk walking, swimming, hiking, or cycling) per week accompanied by two days of resistance training. It’s important to remember that these are the minimum recommendations and clinically significant benefits for people with or at high risk of neurodegenerative diseases will likely require going above and beyond. Patients with more severe motor symptoms that make traditional forms of exercise difficult may benefit from working with an exercise professional for tailored physical activity recommendations.
Mind-Body Therapies
Mind-body therapies for neurodegeneration, like yoga, meditation, and Tai chi, are holistic approaches in neurology that target physical manifestations of neurodegenerative diseases. They also significantly improve mental health, which may be affected especially as the disease progresses.
Yoga
Yoga is an ancient practice that moves the body through physical asanas (postures) and meditation while focusing on the breath. Not only does yoga improve flexibility, strength, and balance, but it also has a major impact on the nervous system through normalizing the stress response. In addition, yoga targets root causes of disease by lowering inflammation, improving digestive, metabolic, and immune system function, and increasing BDNF to help protect the brain.
Mindfulness Meditation
When the nervous system is imbalanced, patients can experience inflammation, poor immune system function, poor digestion, mood changes, depression, and anxiety. Mindfulness meditation involves focusing awareness on the present moment in a non-judgmental way to calm and bring the nervous system back into balance. Meditation has been found to enhance quality of life and psychological well-being in people with AD, ALS, and PD. Additional types of meditation include walking meditation, mantra, and deep breathing.
Tai Chi
Tai chi is a mind-body practice that incorporates slow, repetitive movements along with deep breathing and meditation. In addition to its ability to improve balance for those with PD, Tai chi can target a variety of neurological symptoms by improving cognition, motor function, pain, and quality of life.
Cognitive and Behavioral Interventions
Patients with neurodegenerative diseases often experience poor mental health along with behavior changes that can be disconcerting to the patient and the caregiver. Cognitive and behavioral interventions provide patients and their loved ones with tools to mitigate these symptoms.
Cognitive rehabilitation aims to help patients with neurodegenerative diseases or injuries improve their ability to process and understand information but also allows them to restore critical mental functions. Cognitive therapy for neurodegeneration can include cognitive behavioral therapy (CBT), which teaches patients (and caregivers) how to reframe their thinking to reduce stress and improve coping skills. Other types of cognitive rehabilitation include various recall strategies like mnemonics, chunking, and cueing. Likewise, behavioral interventions in neurology can consist of music therapy, personalized activities, pet therapy, problem-solving therapy, and reminiscence therapy, all of which can help to increase socialization, decrease depression and anxiety, and help patients troubleshoot to solve their problems.
[signup]
Summary
Neurodegenerative diseases are devastating and complex. Our current traditional treatments don’t provide much hope of recovery and often don’t address the genuine impact that these diseases have on the mental health of those who suffer from them.
While we need more research, there are already a myriad of evidence-based integrative therapy options like nutrition, mind-body techniques, physical activity, and behavior therapy, which have the potential to maximize quality of life and possibly even reverse the underlying disease process. Embracing integrative care for neurodegeneration requires an understanding that both traditional and integrative approaches can be used in combination to protect and repair the brain and, most importantly, provide patients with hope.
Lab Tests in This Article






References
- World Health Organization. (2020, Dec 9). WHO Reveals Leading Causes of Death and Disability Worldwide: 2000 - 2019. https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019
- Alzheimer’s Association. (2023). Research Funding. https://www.alz.org/get-involved-now/advocate/research-funding
- Lamptey, R. N. L., Chaulagain, B., Trivedi, R., Gothwal, A., Layek, B., & Singh, J. (2022). A Review of the Common Neurodegenerative Disorders: Current Therapeutic Approaches and the Potential Role of Nanotherapeutics. International journal of molecular sciences, 23(3), 1851. https://doi.org/10.3390/ijms23031851
- Maholy, N. (2023, June 21). Evidence Based Benefits Of Physical Activity For Neurological Health. Rupa Health Magazine. https://www.rupahealth.com/post/evidence-based-benefits-of-exercise-and-physical-activity-for-neurological-health
- Kumar, A., Sidhu, J., Goyal, A., & Tsao, J. W. (2022). Alzheimer Disease. In StatPearls. StatPearls Publishing.
- Blake, K. (2023, Aus 8). Top Nutrients to Reduce Dementia Risk And How To Test Your Nutrient Status. Rupa Health Magazine. https://www.rupahealth.com/post/top-nutrients-to-reduce-your-dementia-risk
- Weinberg, J. (2022, Nov 16). What is the Mediterranean Diet? Rupa Health Magazine. https://www.rupahealth.com/post/4-science-backed-health-benefits-of-the-mediterranean-diet
- Greenan, S. (2021, Oct. 1). These Two Science-Backed Diets Have Been Shown To Reduce Alzheimer’s Risk. Rupa Health Magazine. https://www.rupahealth.com/post/functional-medicine-research-behind-preventing-alzheimers
- DePorto, T. (2023, Jan. 6). Omega 3’s: The Superfood Nutrient You Need To Know About. Rupa Health Magazine. https://www.rupahealth.com/post/omega-3s-the-superfood-nutrient-you-need-to-know-about
- Pisani, S., Mueller, C., Huntley, J., Aarsland, D., & Kempton, M. J. (2021). A meta-analysis of randomised controlled trials of physical activity in people with Alzheimer's disease and mild cognitive impairment with a comparison to donepezil. International journal of geriatric psychiatry, 36(10), 1471–1487. https://doi.org/10.1002/gps.5581
- Ruiz-González, D., Hernández-Martínez, A., Valenzuela, P. L., Morales, J. S., & Soriano-Maldonado, A. (2021). Effects of physical exercise on plasma brain-derived neurotrophic factor in neurodegenerative disorders: A systematic review and meta-analysis of randomized controlled trials. Neuroscience and biobehavioral reviews, 128, 394–405. https://doi.org/10.1016/j.neubiorev.2021.05.025
- Blake, K. (2023, Sept. 11). The Top 6 Integrative Therapy Options For Behavioral Health. Rupa Health Magazine.
- Pagnini F, Marconi A, Tagliaferri A, et al. (2017). Meditation training for people with amyotrophic lateral sclerosis: a randomized clinical trial. Eur J Neurol. https://onlinelibrary.wiley.com/doi/abs/10.1111/ene.13246
- Kwok, J.Y.Y., Choi, E.P.H., Wong, J.Y.H. et al. A randomized clinical trial of mindfulness meditation versus exercise in Parkinson’s disease during social unrest. npj Parkinsons Dis. 9, 7 (2023). https://doi.org/10.1038/s41531-023-00452-w
- Khalsa D. S. (2015). Stress, Meditation, and Alzheimer's Disease Prevention: Where The Evidence Stands. Journal of Alzheimer's disease : JAD, 48(1), 1–12. https://doi.org/10.3233/JAD-142766
- Teeter, L (2023, April 3). Mental Health Benefits of Yoga and Meditation. Rupa Health Magazine. https://www.rupahealth.com/post/mental-health-benefits-of-yoga-and-meditation
- Liu, C., Guo, X., & Chang, X. (2022). Intestinal Flora Balance Therapy Based on Probiotic Support Improves Cognitive Function and Symptoms in Patients with Alzheimer's Disease: A Systematic Review and Meta-analysis. BioMed research international, 2022, 4806163. https://doi.org/10.1155/2022/4806163
- Barman, A., Chatterjee, A., & Bhide, R. (2016). Cognitive Impairment and Rehabilitation Strategies After Traumatic Brain Injury. Indian journal of psychological medicine, 38(3), 172–181. https://doi.org/10.4103/0253-7176.183086
- Kelly, M, and O’Sullivan, M. (2015, July). Strategies and Techniques for Cognitive Rehabilitation. The Alzheimer’s Society of Ireland. https://alzheimer.ie/wp-content/uploads/2019/07/2015-Cognitive-Rehabilitation.pdf
- Scharre, D. (2021, June). Behavioral Approaches in Dementia Care. Practical Neurology. https://practicalneurology.com/articles/2021-june/behavioral-approaches-in-dementia-care
- Blake, K. (2023, June 12). Unlocking The Power Of The Mitochondria: The Mito Food Plan For Optimal Energy And Health. Rupa Health Magazine. https://www.rupahealth.com/post/mito-food-plan
- Maholy, N. (2023, June 29). The Role of Probiotics and Prebiotics in Gut Health: An Integrative Perspective. Rupa Health Magazine. https://www.rupahealth.com/post/the-role-of-probiotics-and-prebiotics-in-gut-health-an-integrative-perspective
- Mohammad, A., Thakur, P., Kumar, R., Kaur, S., Saini, R. V., & Saini, A. K. (2019). Biological markers for the effects of yoga as a complementary and alternative medicine. Journal of complementary & integrative medicine, 16(1), 10.1515/jcim-2018-0094. https://doi.org/10.1515/jcim-2018-0094
- Huston, P., & McFarlane, B. (2016). Health benefits of tai chi: What is the evidence?. Canadian family physician Medecin de famille canadien, 62(11), 881–890.
- Breijyeh, Z., & Karaman, R. (2020). Comprehensive Review on Alzheimer's Disease: Causes and Treatment. Molecules (Basel, Switzerland), 25(24), 5789. https://doi.org/10.3390/molecules25245789
- Stoker, T. B., & Barker, R. A. (2020). Recent developments in the treatment of Parkinson's Disease. F1000Research, 9, F1000 Faculty Rev-862. https://doi.org/10.12688/f1000research.25634.1
- Masrori, P., & Van Damme, P. (2020). Amyotrophic lateral sclerosis: a clinical review. European journal of neurology, 27(10), 1918–1929. https://doi.org/10.1111/ene.14393




%201.svg)







